In children, gastrointestinal infections are the most common cause of ReA. In adults, C. trachomatis is the most common inciting organism.7 Prospective studies of adults with Chamydial infections have shown that 4% to 8% of adults infected will develop ReA.8 Because Chamydial infections are often asymptomatic, the resultant arthritis may not be properly diagnosed as ReA.4 Thus, the true incidence of ReA is largely unknown.
ReA is not considered to be a septic arthritis because cultures from synovial fluid are sterile. Nevertheless, modern polymerase chain reaction (PCR) techniques have demonstrated the presence of bacterial antigens from triggering organisms in the synovium of affected joints.
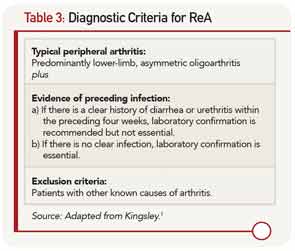
ReA occurs one to four weeks after the inciting infection.4 It usually presents as an acute, painful, sometimes erythematous oligoarthritis (four or fewer joints involved). Arthritis most commonly affects the lower extremities, typically the knees and ankles. In a recent study, enthesitis was the most common musculoskeletal finding in patients with ReA.5 Dactylitis, or sausage digits, may also be present. Back pain and stiffness can develop due to axial involvement. Extraarticular features include fever, painless oral ulcers, urethritis, sterile pyuria, erythema nodosum, and keratoderma blennorhagicum (psoriasiform lesions on the palms and soles that are pathognomonic for ReA).4 During the acute phase of the illness, there are elevated inflammatory markers, thrombocytosis, anemia, leukocytosis, and hypergammaglobulinemia, as were seen in this patient. Autoantibodies including rheumatoid factor, cyclic citrillunated protein, and antinuclear antibodies, are negative.
Pathogenesis
As a type of spondylarthritis, ReA shares many clinical characteristics with the other spondylarthropathies, including a strong association to HLA-B27. However, unlike ankylosing spondylitis, where HLA-B27 is present in about 90% of patients, the prevalence of HLA-B27 in ReA is estimated to be between 30% and 50%.4
The pathogenesis of the spondylarthropathies is not well understood. In patients who are HLA-B27 positive, there is evidence of misfolding of the HLA-B27 protein inside the endoplasmic reticulum. This results in heightened cellular stress that leads to activation of NF-kB and release of proinflammatory cytokines, creating an inflammatory response in the joint.6 This evidence supports the idea that the spondylarthropathies are within the spectrum of polygenic autoinflammatory diseases, in which local factors activate the innate immune system to cause tissue-specific inflammation. This is in contrast to autoimmune diseases such as lupus, in which disease-specific autoantibodies, self-reactive lymphocytes, and enhanced activation of the adaptive immune system are key to the pathogenesis of the disease.