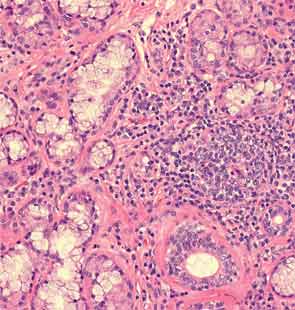
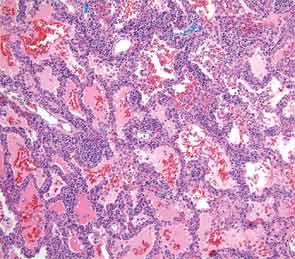
An extensive infectious disease workup for viral infections, tuberculosis, fungi, and bacteria was negative. A transbronchial biopsy was negative for any infectious etiology or granulomas. Histopathology revealed nonspecific interstitial pneumonitis (NSIP) pattern. The otolaryngology service was consulted for a minor salivary gland biopsy, which was subsequently reported as being consistent with Sjögren’s syndrome (SS) based on more than one focus of more than 50 lymphocytes per 4 mm2 (see Figure 3). A surgical lung biopsy confirmed NSIP (see Figure 4); fibrosis was absent. At this time, the anti-Jo-1 antibody was reported as positive at 7.9 (0–0.9 AI)). The serum aldolase level was elevated at 9.4 (1.5–8.1 U/L).
A diagnosis of antisynthetase syndrome with subclinical SS—based on positive serologies and biopsy in the absence of sicca symptoms—was made. The patient was placed on oral prednisone at 1 mg/kg and hydroxychloroquine 200 milligrams twice daily. After three days of treatment, he had a remarkable response and his joint symptoms resolved. At three months of follow-up, he was on prednisone 40 mg, had no complaints, and his PFT and chest radiograph had normalized. He was started on methotrexate 10 mg weekly to allow for steroid taper.


Discussion
Rheumatologists are often asked to evaluate patients presenting with interstitial lung disease (ILD) in association with a positive ANA or RF, joint, or musculoskeletal symptoms. This case highlights one such typical scenario. The initial concern was for an ANCA-associated disease based on the presence of aural symptoms, hemoptysis, lung disease, and arthritis. However lack of ANCA antibody positivity, absence of any bony erosion on sinus imaging, and subsequent biopsy without histological evidence of vasculitis merited a diagnostic reevaluation.
Antisynthetase syndrome is a systemic autoimmune syndrome characterized by a variable combination of ILD, myopathy, fever, joint involvement, and mechanic’s hands with a reported prevalence of 1.5 per 100,000. Its hallmark is the presence of antibodies directed against aminoacyl-transfer RNA synthetase of which the most frequent is the anti-Jo-1 antibody that accounts for about 80% of all cases of antisynthetase syndrome.1 Other relatively common antibodies include anti-PL-7 and anti-EJ.2 Anti-Jo-1 antibodies are present in about 30% of patients presenting with myositis and it is in the setting of myositis that these antibodies are usually tested to diagnose antisynthetase syndrome. ILD, however, is the most frequently occurring manifestation of antisynthetase syndrome and is reported in 75% to 89% of all cases.3 Lung involvement is the most important determinant of prognosis.