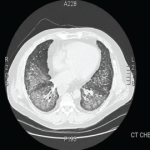
ILD is the most frequent manifestation, and in some cases the sole one, of antisynthetase syndrome.3 In about 20% of cases, the plain radiographs are read as normal, despite pulmonary involvement. When this diagnosis is being considered, high resolution CT scanning of the chest should be performed. Common findings include bilateral basal consolidations, diffuse patchy ground-glass opacities and subpleural prominence. On lung biopsy, NSIP is the most common pattern seen, although it is not specific for antisynthetase syndrome. Biopsy is important to rule out infections, granulomatous diseases, and vasculitis. It can also determine whether there is lung fibrosis. The absence of fibrosis predicts a better response to therapy. Although hemoptysis is not a regular feature of pulmonary involvement in antisynthetase syndrome, it has been reported.
Joint symptoms are more common in anti-Jo-1 positive patients and can mimic common inflammatory arthritides.4 RF, for example, can be positive in 10% to 20% of subjects with idiopathic pulmonary fibrosis (IPF). Patient with IPF can also have arthralgias, and it is important to look for secondary clues to an underlying connective tissue disease (CTD) before labeling any disease as idiopathic.
The lack of a unifying diagnosis, positive family history for a CTD, and absence of any identifiable environmental exposure or infection in the setting of a strongly positive SSA/SSB prompted the minor salivary gland biopsy, despite the fact that the patient did not have typical symptoms or the CT findings expected in SS. As noted, the biopsy was consistent with SS.
The utility of obtaining salivary gland biopsies in such settings can be debated, owing to false-positive rates and the significant variability in their interpretation. However, one study evaluating ILD patients without an underlying cause found 34% of patients having a biopsy suggestive of SS, of which 23% were negative for ANA, SSA, and SSB.5 About 23% of those with a positive biopsy denied sicca symptoms. The authors postulated that SS was subclinical in these patients. They also felt identification of a patient with an underlying disease, in this case SS—whether clinical or subclinical—conferred a better prognosis than the diagnosis of idiopathic ILD. It is difficult to say whether a salivary gland biopsy should be considered in an otherwise asymptomatic patient with an idiopathic ILD. SSA is frequently seen in association with anti-Jo-1, and evidence suggests an increased severity of ILD in patients with SSA positive antisynthetase syndrome.6
The lack of muscle symptoms in this patient contributed to the delay in arriving at the final diagnosis. It is important to note that myositis may not be one of the presenting features in antisynthetase syndrome. In one series of ILD patients with anti-Jo-1 antibodies, myositis was present in only 31% at initial presentation.3 The anti-Jo-1 presence can precede clinical myositis by years.