Although the patient remained asymptomatic, approximately one year later, a new chest CT study showed enlargement of existing mediastinal and hilar lymph nodes and new additional mediastinal nodes. Etanercept was discontinued due to a suspicion that it may be related to the relapse of sarcoidosis, and sulfasalazine was started in conjunction with a prednisone taper. Two months after discontinuation of etanercept, another chest CT showed decrease in size of the subcarinal lymph node and the right paratracheal nodes. PFTs showed a stable vital capacity of 77%, DLCO 59%, and forced expiratory volume (FEV1) was normal at 86% of predicted.
While on sulfasalazine, the patient was able to cope with his skin and joint disease. Intermittent joint flares were treated with intraarticular corticosteroid injections while psoriasis flares were treated with topical corticosteroids.
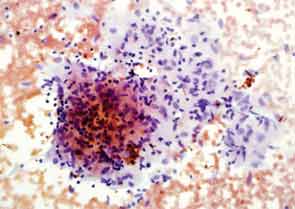
Two years later, the patient developed dyspnea on exertion and a nonproductive cough. PFTs showed a decrease in the vital capacity to 71% and DLCO to 55% of predicted. FEV1 decreased to 77% of predicted. This time, chest CT imaging showed improvement in mediastinal and hilar adenopathy, but there was an increase in parenchymal manifestations of sarcoid disease with perilymphatic distribution of nodules in upper lobes of lungs bilaterally. A bronchoscopy with biopsy was performed and excised tissue was consistent with noncaseating granulomas (see Figure 2). Repeat AFB and fungal cultures were negative. Serum calcium was 9.1(8.3–10.5 mg/dl) and angiotensin-converting enzyme (ACE) 49 (9–67 U/L). Because of his poorly controlled sarcoidosis, the patient was started on infliximab 300 mg intravenously every eight weeks. Four months later, the patient was free of respiratory, skin, and joint symptoms. He continues to do well and denies any dyspnea on exertion or other systemic manifestations of sarcoid disease while on infliximab. The pulmonary function tests are stable. The chest radiograph appearance has improved and his exercise tolerance improved.
Case #2
A 32-year-old white male with a history of psoriasis diagnosed in 1998 presented to rheumatology clinic in 2007 with a two-week history of pain and swelling in his hands, ankles, shoulders, and low back. Physical exam revealed erythematous plaques covered by silvery white scaly lesions over his lower extremities and there was onycholysis in several fingernails. There was an asymmetric synovitis involving his wrists, metacarpophalangeal and proximal interphalangeal joints, and both ankles. He was diagnosed with psoriatic arthritis and started on prednisone and methotrexate. A baseline CXR was unremarkable. After one month of treatment with methotrexate, the dose was reduced because of elevated serum transaminases, and the prednisone dose was increased due to persistent arthritis. This regimen offered only moderate disease control and it resulted in significant weight gain. Adalimumab 40 mg subcutaneously every other week was initiated.



