Case 1
A 27-year-old Caucasian woman previously in good health presented to the emergency department (ED) with three months of progressive fatigue, shortness of breath, paroxysmal nocturnal dyspnea and orthopnea. She also described left flank pain, left frontal neck and upper back pain, left arm claudication and frequent left-side headaches. She had an episode of complete loss of vision in her left eye lasting a few seconds three months prior to admission, but she did not seek medical attention at the time. Her progressive shortness of breath prompted her ED visit.
A chest computed tomography (CT) scan was performed to evaluate for a pulmonary embolus, but instead it revealed dilation of the ascending aorta and a 3.9 cm wide fusiform aneurysm of the descending thoracic aorta. Her blood pressure was 98/49 mmHg in her right arm, 88/36 mmHg in her left arm, 133/26 and 135/26 mmHg in her right and left legs. Her physical exam was significant for a IV/VI diastolic murmur loudest at the right upper sternal border, a barely palpable left carotid pulse, and weak left axillary, brachial and radial pulses. The rest of her vascular exam was normal.
Her basic laboratory tests were unremarkable except for an anemia with a hemoglobin of 11.9 (reference 12.0–16.0 g/dL). A high-sensitivity C-reactive protein (hs-CRP) was 19 (reference <7.4 mg/L) with an erythrocyte sedimentation rate (ESR) of 5 (reference <25 mm/hr). A transesophageal echocardiogram revealed thickening of the ascending aorta, severe aortic insufficiency with a flail right cusp, aortic root dilation and thickening of the valve. Her left ventricular ejection fraction was 35%.
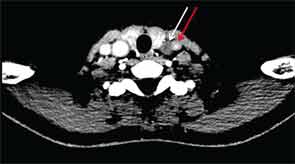
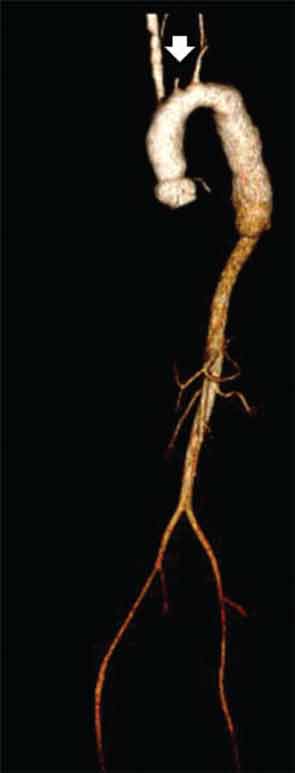
CT of the neck showed complete occlusion of left common carotid artery immediately above the stump (see Figure 1) and complete occlusion of the left internal carotid artery with retrograde filling via the circle of Willis. Significant wall thickening and multiple areas of irregularity and dilatation were seen in the right innominate, right common carotid and left subclavian arteries. A CT angiogram (CTA) of the chest, abdomen and pelvis demonstrated a dilated ascending and descending thoracic aorta with a maximum dimension of 4 cm with concentric wall thickening extending to the midthoracic aorta (see Figure 2). There was no involvement of her abdominal aorta.
The patient was given a pulse dose of glucocorticoids with methylprednisolone 500 mg intravenous daily for three days with improvement in the strength of her left brachial and radial pulses over the course of treatment. She was also initiated on aspirin 81 mg daily and azathioprine 50 mg daily, which was further titrated as an outpatient. After the glucocorticoid pulse, the dose was reduced to prednisone 1 mg/kg/day. Aortic valve replacement was deferred in order to treat the inflammatory vascular process and because she was well compensated clinically. She returned a month later and continued to have stable heart failure symptoms, although she had episodes of left-side amaurosis fugax, lasting less than 15 seconds. Her glucocorticoid dose will be tapered in anticipation of an aortic valve replacement.
Case 2
A 31-year-old Hispanic woman presented to the hospital with hypertension and renal failure.