 Like the medical profession itself, the education of doctors serving in rheumatology fellowships across the nation marches on despite the unexpected hurdles posed by the COVID-19 pandemic.
Like the medical profession itself, the education of doctors serving in rheumatology fellowships across the nation marches on despite the unexpected hurdles posed by the COVID-19 pandemic.
Practice Changes
“The pandemic has changed the way our fellows see patients; we are now seeing almost all patients using telemedicine,” says Bonita Libman, MD, FACR, FACP, fellowship program director for the Division of Rheumatology and Clinical Immunology at the University of Vermont Larner College of Medicine, Burlington, Vt.
Similar scenarios are playing out across the nation as fellowship trainees adjust to fewer in-person visits and hold many more consultations via telephone or video communication. Program directors and their trainees continue to care for patients while navigating governor-issued, stay-at-home orders and the need for six feet of physical distance between people to limit spread of the virus.
Training Changes
For didactic education, faculty and students still meet, but not in person. Many professors use the Zoom platform to conduct online lectures and conferences, often with students viewing from the comfort of their own homes.
“This [approach] worked out very well,” says Dr. Libman. “In fact, we had more participation in virtual conferences than when people had to show up for them in person.”
Other fellowship directors say they too have seen lecture attendance increase since it became necessary to move didactic education out of the traditional classroom and into online video rooms. Often, it’s easier to open a laptop from home and get right to it—no driving, traffic jams or other distractions.
“Our lecture series has, thankfully, been relatively preserved despite the COVID-19 pandemic,” says Jason Kolfenbach, MD, associate professor of medicine and rheumatology fellowship program director at the University of Colorado Anschutz Medical Campus, Aurora. “We were kind of set up for that because we have a faculty member in our division, Duane Pearson, MD, who has [already] been using the Zoom platform for education of primary care providers in rural areas.”
Online Training Challenges
Starting on March 11, all weekly lecture series transferred to Zoom for Dr. Kolfenbach’s fellowship program, which covers a three-hospital system stretching across the Denver metropolitan area.
“The biggest change for us has been the clinical training,” says Dr. Kolfenbach, noting that his rheumatology trainees have various specialty rotations and some have been stopped as a result of pandemic pressures and priorities.
“The pulmonary division is knee deep in the clinical management of hospitalized and ventilated patients, and our surgical colleagues in orthopedics have stopped elective procedures. So the ability of some specialties to remain engaged with these outpatient clinics is less than it used to be,” says Dr. Kolfenbach.
“Obviously, we are trying to be respectful of that, and as a result we’ve hit the pause button on some of these clinical rotations,” he notes. “In the rheumatology clinic, our volume has dropped some, as well. We’ve converted probably 90% of outpatient visits to telemedicine, reserving in-person visits for those who still require the traditional face-to-face encounter.”
Kristine M. Lohr, MD, MS, professor of medicine, rheumatology division chief and director of the rheumatology fellowship program at the University of Kentucky School of Medicine, Lexington, says the new social distancing rules mean she is the only one in the rheumatology office most of the time. Conferences initially held in large rooms to accommodate physical separation quickly shifted to video communication on Zoom.
“Our fellows stay home to study, except for the fellow on call for inpatient consults or weekends. We appreciate the ACR’s ViRL conferences and Dr. Jack Cush’s RheumNow [presentations],” Dr. Lohr says.
“What the fellows miss is the opportunity to do procedures, [because] patients aren’t coming in for visits,” she says. “The number of COVID-19 patients in our hospital has not reached the point [at which] providers and staff are being called into service.”
When it comes to adopting new technology, the younger you are, the smoother the sailing, say some program directors. Incorporating the technological aspects of telemedicine into the clinic presented a steep learning curve for Dr. Libman and a shining moment for her students.
“Our fellows are technology savvy, so they quickly figured out how to see patients, with the fellow seeing the patient first, presenting [patient information] to the attending, then creating a three-way call for the attending to review and confirm the plan [with the patient],” says Dr. Libman.
“The most surprising part of this [situation] was how easy and enjoyable it was to use telemedicine [after] we understood the technology—and the coding and billing requirements,” she says.
At the University of Colorado, fellows review patient charts the week before a scheduled visit to identify which patients are appropriate for a telemedicine visit. Virtual visits via Epic’s electronic medical records system allow the fellows to work from home. They receive an electronic notification that the patient and staff are online and ready for the appointment. In minutes, the patient chart and live pictures of each person show up on a screen the fellow operates from a computer or cell phone.
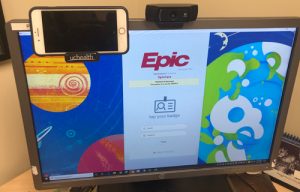
Dr. Kolfenbach uses multiple screens at his desk for telemedicine appointments and meetings with fellows and others in the rheumatology department.
“As a faculty [member], I can join into that [session] remotely, as well. Up to five people can be in the virtual room, so at any time the patient, medical assistant, medical translator, fellow and faculty member can all be engaged in clinical care with no one actually in the physical rheumatology clinic,” says Dr. Kolfenbach.
Some medical needs, such as infusions, obviously cannot be accommodated by phone or telemedicine. Clinics remain open for rheumatology patients who require in-person care. “We still see patients in person if the clinical need mandates it,” says Dr. Kolfenbach. Although visits have decreased in part because some patients cancel appointments, “our doors are not shut,” he says.
Dr. Kolfenbach sees the recent adjustments as stopgap measures to keep patients as stable as possible during the challenges of the pandemic. It’s important for rheumatology fellows to gain experience with the hands-on nature of the specialty, such as examining a patient for swollen joints.
“Our job as rheumatologists, especially in patients with inflammatory joint disease, can be heavily influenced by exam findings,” says Dr. Kolfenbach. “An exam can be performed in a telemedicine visit, but there are limitations. If the pandemic continues to keep patients away for months on end, I worry that care could be impacted for patients who miss out on the opportunity to receive a thorough physical exam.
“We all learn from doing things by repetition, and if clinical volume is down, then that’s fewer opportunities to learn how to take care of somebody who has a chronic illness,” he says. “Our program is tracking patient numbers for the fellows, and we will think of creative ways to provide more opportunities if this is sustained.”
Well-being
Adjusting to technological changes that improve safety for both patients and staff is easier to achieve compared with the ongoing effort to keep everyone feeling well physically, mentally and emotionally. The separation from ordinary, everyday interaction and routine can lead to feelings of isolation, notes Dr. Libman.
“I try to keep lines of communication open and ask how people are doing,” says Dr. Libman. “Even small talk or a brief hello can be a powerful way to connect with and support each other.”
Aside from career challenges for fellows, the pandemic takes a toll on personal lives, too.
“One first-year fellow took her vacation in her apartment, instead of visiting the beach—definitely a disappointment,” Dr. Lohr says. “She’s concerned about her boyfriend, a neurology fellow in Michigan [who was] called on to cover internal medicine patients.
“Since the other first-year fellow’s daughter interrupts her studying, she studies in our administrative assistant’s office,” she adds. “Her husband is finishing his degree in another state, but visited for a while. Both first-year fellows are in the process of job seeking, but obviously not traveling.”
On the bright side, being able to study from home has reduced childcare costs for a pair of second-year fellows training with Dr. Lohr. “Their older daughter is restless staying indoors, so they visited my back pasture to walk outdoors,” she says.
Catherine Kolonko is a medical writer based in Oregon.






