The best way to understand complex systems is with a holistic approach: viewing the system dynamics in its entirety and observing its interactions with the environment. Complexity theory provides a scientific foundation for holism. Rather than opponents, holism and reductionism should be regarded as complementary scientific tools; both perspectives are needed for a proper account of reality.
Complexity theory may have important clinical implications. The main homeostatic systems of the human body are complex. Static blood tests or imaging techniques cannot detect dysfunction of such homeostatic systems.
Autonomic Nervous System: Prototype of Complex Adaptive System
The best example of a complex adaptive system in the human body is the autonomic nervous system (ANS).7 The fundamental role of the ANS in health maintenance is represented by the fact that it regulates vital signs.
The performance of the ANS cannot be appreciated with linear tools. There is a novel, nonlinear procedure based on computer calculations called heart rate variability analysis. This method demonstrates that young healthy individuals have flexible sympathetic–parasympathetic harmonious interactions. With disease or aging, the system becomes rigid, thus losing its complexity.8 In other words, disorder can be healthy while uniformity can lead to disease.
Complexity Loss in Fibromyalgia
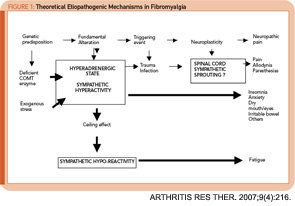
Several groups of investigators have shown that FM patients have decreased heart rate variability. This alteration can be interpreted as sign of “decomplexification” of the ANS with persistent rigid circadian sympathetic hyperactivity. It has been proposed that such alteration explains FM multisystem features as shown in Figure 1 (right).7
Rigid sympathetic hyperactivity can lead to aberrant neuroplasticity, establishing abnormal connections between the sympathetic nervous system and the nociceptive system. Animal models have identified the dorsal root ganglia as an important short-circuit site. Triggering events for FM could be physical or emotional trauma as well as different types of infections. The resulting clinical syndrome is a sympathetically maintained neuropathic pain syndrome (pain, allodynia, and paresthesias). Sympathetic hyperactivity may cause other FM symptoms not related to pain.7
Degraded environment may explain the high prevalence of FM at present. Industrialization has disfigured circadian cues, diets, exercise, and working conditions among many other variables. Susceptible individuals such as women with deficient catecholamine-handling enzymes would be more prone to become ill. FM can therefore be viewed as a failed attempt of our main complex system to adapt to a hostile environment.
Of course, much more research is needed to confirm or amend this model.
Holistic Treatment
As the experience of many providers shows, in FM, the conventional (linear) medical visit in which the patient acts as passive consumer of medication and advice is likely to be ineffective. Instead, a bio-psycho-social approach is recommended. Holistic interventions are too diverse to be fully covered in this article. Table 1 (above) outlines those procedures having scientific and/or a group of experts’ support.9 Most of the discussed methods have shown to improve autonomic tone.
Conclusion
FM will not disappear by ignoring its existence or demeaning its perplexing features. To the contrary, degraded modern lifestyles are likely to increase its prevalence and make FM an even greater problem.