SAN DIEGO—Fibrosis affects all organ systems, but isn’t always systemic sclerosis. Experts on less common forms discussed patient presentations, diagnosis and treatment at the 2017 ACR/ARHP Annual Meeting in San Diego on Nov. 6.
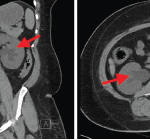
Retroperitoneal Fibrosis
Formerly called Ormond’s disease, retroperitoneal fibrosis (RPF) is usually an IgG4-related disease, but has some unique characteristics, said John H. Stone, MD, MPH, director of clinical rheumatology at Massachusetts General Hospital in Boston. New classification criteria for IgG4-related disease will be released in 2018. When IgG4 related, RPF tends to affect the area around the aorta. It may affect the submandibular gland, kidney or pancreas, too.
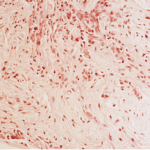
He shared biopsy results of an RPF patient with storiform fibrosis typical of IgG4 disease. “The fibrosis has a swirling pattern to it. Lymphoplasmacytic infiltrate is enmeshed in this fibrosis,” he said. Storiform derives from the Latin word storea or woven mat. The patient also had high eosinophils, and many of his plasma cells stained positive for IgG4.
RPF often causes obliterative phlebitis, he said. One of the patient’s veins was “completely destroyed, just trashed, by the inflammation. Lymphoplasmacytic infiltrate moved in and destroyed it, so you can’t even see it without an elastin stain.”
Biopsy may be challenging as inflamed tissue is typically near the aorta and hard to reach, he said. “Often, only a small piece of tissue can be removed. You have to be careful about how you interpret what you see from a small piece of tissue. Finding overwhelming fibrosis with no footprints of the inflammation that led to that pattern is also problematic in interpretation.” In highly fibrotic tissue, stain to see if most of the plasma cells are IgG4-positive. Exclude malignancy as well, he said.
RPF is not always IgG4-related, and the association between it and other disease on this spectrum is still unclear, said Dr. Stone.1 Fewer organs are involved, often just those in the retroperitoneum. Although some patients have very high IgG4 levels, others have normal IgG4 serology.2 RPF seems to fall on the more fibrotic end of the spectrum of IgG4-related diseases, rather than the inflammatory end.
“Treatment responses are often less profound, but patients with RPF can respond and even have excellent responses. Even if their fibrosis doesn’t melt away with treatment, they can have enormous improvement in their quality of life. It’s wrong to think of these patients as having burnt-out disease that won’t respond to treatment,” he said, and finds that corticosteroids are usually very effective. Imaging may suggest fibrosis or inflammation has greatly improved with therapy in some, but not all, patients.