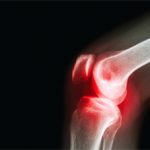
Try this test on one of your patients to really appreciate the effect of foot position on a symptomatic knee. Most people with arthritis of the knees will also have some pain when doing the simple squat test I mentioned above. However, in many instances, when this test is repeated with some small wedges (like simple doorstops) under the forefoot and rear foot, (so that the patient is more supinated and his or her knees are more vertically aligned), the patient can usually squat easier and with less pain. The reduction in symptoms occurs in many instances because you are now allowing the joint to function on some remaining cartilage laterally. These results are improved further when a small lift (1/4 inch or more) is placed under a short leg.
I fully appreciate that we are all under severe time constraints with our patients. However, I believe that, in most cases, improvements (sometimes dramatic and immediate) can be made by incorporating brief structural evaluations into routine examinations. You will also find less need for medications and surgery. The goal of this article is not to make you a specialist in biomechanics—I’m certainly not. Rather, I would like to:
- Help you appreciate the important role of pathomechanics in arthritis of the weight-bearing joints;
- Share some simple ways to evaluate structural abnormalities and the need for correction;
- Suggest a basic treatment plan; and
- Help you determine the effectiveness of therapy.

Steps for a Therapeutic Approach to Pathomechanics
- Accept the premise. As I mentioned at the onset, the first step in implementing this treatment plan is to appreciate fully the role of patholmechanics in OA—and there is much supportive data (see “Research Overview,” p. 33).
- Identify the presence of structural abnormalities. While a patient is standing, notice if one arm is longer or one shoulder is higher. See if one knee is more flexed, one hip seems higher, or one foot is flatter than the other. Watch your patients walk. Ask them to squat and see if their knee (or knees) internally rotates. Most importantly, while they are seated, place their feet (in subtalar neutral) directly under their knees and notice the difference when they stand up, as described above. The critical care element here is to hold this optimal, subtalar neutral, non–weight bearing foot position, because this will dramatically affect all weight-bearing joints.
- Make a good physical therapist part of the team. Focus must be redirected to finding and correcting the specific structural abnormalities that are the real causes of OA (e.g., leg length differences). Once the joints are aligned, range of motion and strength and conditioning exercises, as well as braces and other therapeutic modalities, will be far more effective.
- Limit patient weight-bearing activity. Doing this initially can be quite helpful because using a joint in poor alignment can far outweigh the positive benefits of exercise. Once alignment is accomplished, activities can often be resumed, often with far more effectiveness.
- Help patients lose excessive weight. Weight is an important secondary factor in OA.
- Prescribe custom foot orthotics. Orthotic is a very broad, generic term that implies “something” that is being used to support the arch. Much confusion exists about terminology and classifications. Strictly speaking, the more correct term is orthosis, from the Greek for “straight, upright, or correct.” The implication of the derivation is the most important thing: your patients should be standing straight and upright when on their devices, and not be as pronated as they are without them.
Simply having foot orthotics is meaningless. As with a set of prescription eyeglasses, the precision with which orthotic corrections are made is directly related to decreasing symptoms and improving function. Once you begin looking at correction, you will see that, many times, patients have very little correction at all. One of the biggest reasons for this is improper casting technique. There is usually a significant difference in a patient’s foot when on and off weight bearing (see Figure 2, below). In my opinion, impressions that are taken with the patient standing can only capture the foot in its pathological, usually maximally pronated position. I believe that a device made from such an impression is far less effective than one produced from a non–weight bearing cast.