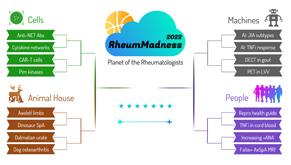
 Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The more your picks match those of our Blue Ribbon Panel of rheumatologists, the more points you get. Learn more about the panel and how the brackets work online.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn more on the RheumMadness website.
Region: Machines Team: PET CT in Large Vessel Vasculitis
PET in LVV is the team to watch. A study by Grayson et al. from the U.S. National Institutes of Health forms our team’s solid foundation, with a single-center, prospective longitudinal cohort study evaluating 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET) in large vessel vasculitis (LVV) against a group of vasculitis-mimicking comparators.1 Adult patients underwent FDG-PET combined with computed tomography (CT), and patients aged 18 and younger underwent whole body FDG-PET combined with magnetic resonance imaging (MRI).
In this study, 56 patients with LVV (30 with giant cell arteritis [GCA] and 26 with Takayasu arteritis) and 59 comparators (35 with hyperlipidemia, 17 with disease-mimicking LVV and 7 healthy controls) participated over a three-year period. During the study, each comparator underwent a single FDG-PET scan and each LVV patient underwent FDG-PET scan at entry and six-month intervals, with preceding clinical disease activity assessment by history, physical and laboratory evaluation.
 In total, 111 FDG-PET scans were completed for 56 patients with LVV. Of the 40 patients with clinically active LVV, 34 had FDG-PET scans consistent with active vasculitis. Interestingly, 41 FDG-PET scans of the 71 patients with LVV in clinical remission were read as active vasculitis.1
In total, 111 FDG-PET scans were completed for 56 patients with LVV. Of the 40 patients with clinically active LVV, 34 had FDG-PET scans consistent with active vasculitis. Interestingly, 41 FDG-PET scans of the 71 patients with LVV in clinical remission were read as active vasculitis.1
The non-LVV comparator group had 10 of 59 FDG-PET scans that read as active vasculitis, resulting in FDG-PET 85% sensitivity and 83% specificity in distinguishing clinically active LVV and specificity of 42% in distinguishing clinically active vs. remission LVV. Multivariate modeling showed a positive FDG-PET scan was more likely in clinically active disease, short disease duration, lower body mass index (BMI) and lower doses of prednisone.
Part of our underdog team’s brilliance is its incorporation of the PET Vascular Activity Score (PETVAS), a novel scoring system designed to provide qualitative assessment of arterial uptake in four aortic segments and 11 branch arteries compared with liver uptake on FDG-PET scans (Note: This analysis was only performed for FDG-PET-CT). Each segment receives a 0–3 score that is summed to create the PETVAS score. Higher scores, which are indicative of increased vascular inflammation, were felt to correlate well with visual interpretation of active vs. inactive vasculitis on FDG-PET-CT scans (P<0.0001). One highlight: A PETVAS score greater than 20 predicted a clinical relapse over a median time frame of 15 months in patients who were otherwise thought to be in clinical remission (i.e., 55% of patients with a score of >20 had a clinical relapse compared with 11% of patients with a score of <20 who had a clinical relapse).
With the ball in their court, Quinn et. al compared FDG-PET to magnetic resonance angiography (MRA) in patients with LVV and found FDG-PET superior in reliably detecting disease activity and that FDG-PET enhancement was more likely than MRA to correlate with active clinical disease assessment. However, MRA was superior in detecting the extent to which disease was involved in vascular territories due to its ability to detect arterial wall and lumen abnormalities.2 When comparing FDG-PET to computed tomography angiography (CTA), FDG-PET was more sensitive and detected more involved arterial segments than CTA.3
FDG-PET is not disease specific but can detect inflammatory, infectious and malignant conditions. Thus, it needs to be cautiously interpreted. A minimum of 60 minutes is recommended from intravenous 18F-FDG administration to image collection for adequate tracer distribution.4 Additionally, our potential Achilles heel is glucocorticoid use, a cornerstone of LVV treatment because it reduces metabolic cell activity and 18F-FDG uptake, which can result in a significant decrease in signal after three days of treatment.5
Implications
FDG-PET is a cutting-edge modality with the potential to change the game of LVV. It demonstrates impressive sensitivity and specificity in capturing active LVV, allowing quantification of activity with PETVAS and predicting the risk of relapse for patients thought to be in remission.
In the future, we hope to see standardization of FDG-PET protocols for LVV, qualitative scoring and additional prospective longitudinal studies using FDG-PET scans at time of diagnosis. Then, serial monitoring to see if abnormalities on FDG-PET scans truly correlate with poor, long-term clinical outcomes.
Chances in the Tournament
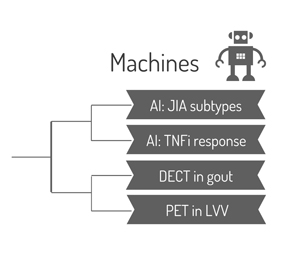
FDG-PET in LVV opens the tournament against DECT in Gout, which looks like a match-up of two similarly minded teams whose game plans revolve around a vision—or image—of outside to inside to score the buckets (diagnosis). FDG-PET in LVV has an honorable mention in conference play (see the 2021 vasculitis guidelines), and DECT in Gout’s defense of preventing joint aspiration pales in the intense face of FDG-PET in LVV’s defense against the biopsy of a large artery.
FDG-PET in LVV’s future in the tournament is brighter than the vessels it images because of a team composition of youngsters with Takayasu arteritis and experienced vets with GCA. FDG-PET in LVV is the ultimate team player, bringing together rheumatologists, radiologists and nuclear medicine to develop the FDG-PET game plan.
However, the technology may still be a few years away from winning it all because of questions regarding its scouting ability—or FDG-PET’s role in monitoring and managing LVV. Unfortunately, it may be derailed from bringing all it has to offer to the table by insurance companies and cost.
Sean Carter, MD, is a first-year fellow in the Medical University of South Carolina Rheumatology Fellowship Program, Charleston.
Jessica English, MD, is a first-year fellow in the Medical University of South Carolina Rheumatology Fellowship Program, Charleston.
Brad Collins, DO, is a first-year fellow in the Medical University of South Carolina Rheumatology Fellowship Program, Charleston.
Ana Tucker, MD, is a second-year fellow in the Medical University of South Carolina Rheumatology Fellowship Program, Charleston.
Jen Schmidt, MD, is a second-year fellow in the Medical University of South Carolina Rheumatology Fellowship Program, Charleston.
Whitney Elg-Salsman, DO, is a third-year fellow in the Medical University of South Carolina Rheumatology Fellowship Program, Charleston.
Faye Hant, DO, is fellowship director of the Medical University of South Carolina Rheumatology Fellowship Program, Charleston.
References
- Grayson PC, Alehashemi S, Bagheri AA, et al. 18F-fluorodeoxyglucose-positron emission tomography as an imaging biomarker in a prospective, longitudinal cohort of patients with large vessel vasculitis. Arthritis Rheumatol. 2018 Mar;70(3):439–449.
- Quinn KA, Ahlman MA, Malayeri AA, et al. Comparison of magnetic resonance angiography and 18F-fluorodeoxyglucose positron emission tomography in large-vessel vasculitis. Ann Rheum Dis. 2018 Aug;77(8):1166–1171.
- de Boysson H, Dumont A, Liozon E, et al. (2017). Giant-cell arteritis: Concordance study between aortic CT angiography and FDG-PET/CT in detection of large-vessel involvement. Eur J Nucl Med Mol Imaging. 2017 Dec;44(13):2274–2279.
- Tawakol A, Migrino RQ, Bashian GG, et al. In vivo 18F-fluorodeoxyglucose positron emission tomography imaging provides a noninvasive measure of carotid plaque inflammation in patients. J Am Coll Cardiol. 2006 Nov 7;48(9):1818–1824.
- Nielsen BD, Tønder Hansen L, Keller KK, et al. Attenuation of fluorine-18-fluorodeoxyglucose uptake in large vessel giant cell arteritis after short-term high-dose steroid treatment—a diagnostic window of opportunity [abstract: 3182]. Arthritis Rheumatol. 2016 Oct;68[suppl 10].
 Experience All of RheumMadness
Experience All of RheumMadness
During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports. Check out the reports from each region:
Region: Cells
Region: Animal House
Region: Machines
Region: People
• False Positive MRI in Axial SpA
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The winner of each match-up is decided by a seven-member Blue Ribbon Panel of rheumatologists. The panel will vote based on which topic they think is most important to patients, providers and researchers—both now and in the future. The more your picks match those of the panel, the more points you get. The tournament results will be released in four rounds from March 26–April 4. Prizes will be given to participants with the top scores in the following categories: 1) attending/APP, 2) fellow and 3) resident/medical student. The prize is a custom RheumMadness coffee mug and a lifetime of bragging rights.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn on the RheumMadness website.



