The ACR has published the “2010 Recommendations for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis.”1 An update to the 2001 recommendations, these new guidelines take into account new therapies and updated diagnostic approaches that have been developed since the 2001 recommendations were published, as well as new data on the therapies mentioned in the 2001 publication.
Jennifer M. Grossman, MD, principal investigator and coauthor of the recommendations, tells her patients that a glucocorticoid “is a good drug, but it’s also a bad drug at the same time. Most of us had thought that 2.5 mg per day was a pretty safe dose, but there are patients taking that dose who should be getting a prophylactic medication for osteoporosis.”
The 2010 recommendations make it clear that any dose of glucocorticoids for management of inflammatory conditions can be associated with significant morbidity and mortality. Decline in bone mineral density can begin within the first three months of use, will often peak by six months, and then will continue with ongoing use.
“Patients on glucocorticoids fracture at a higher bone mineral density than patients not on glucocorticoids,” says Dr. Grossman, associate clinical professor of medicine in the department of rheumatology at the David Geffen School of Medicine at the University of California, Los Angeles. “We should not be relying just on bone mineral density when deciding whether to use pharmacologic therapy with these patients,” she notes.
The need to assess bone health beyond bone mineral density is an important change from the 2001 recommendations. The 2010 recommendations “try to incorporate different aspects that raise a patient’s threshold of fracture risk, which is really important in these complicated rheumatology patients,” she says.
Assess Risk Beyond FRAX Score
Use of the Fracture Risk Assessment Tool (FRAX) can help determine a patient’s fracture risk, but it can give an incomplete assessment. “One of the factors not captured by FRAX is glucocorticoid dose. Instead it is listed as ‘ever’ or ‘never’ used. If you have someone on a much higher dose, such as 20 mg daily, you may want to consider osteoporosis prevention therapy in that patient,” regardless of their score on FRAX,” Dr. Grossman says. (See “Making of the Guidelines” for more on FRAX.)
Another issue with only using the FRAX score is that the degree of fracture risk calculated by FRAX is based on bone density value for the hip. Because glucocorticoid-treated patients frequently lose bone mass in the spine before the hip, a FRAX score may underestimate their risk of fracture. One new recommendation is that physicians consider ordering a vertebral fracture assessment for patients initiating or receiving 5 mg or more of prednisone daily because patients are often unaware that they have had a vertebral fracture.
“If you picked up a vertebral fracture in someone who has a T score of -0.8, that patient should be treated because a vertebral fracture is one of the major risk factors for future fractures,” Dr. Grossman says. Getting reimbursement for a vertebral fracture analysis can be a problem, one she hopes will change given these new recommendations. “Since a third of all vertebral fractures are clinically apparent, you might end up treating a third more patients if you were able to do this analysis,” she notes.
Several other factors can indicate an increased fracture risk for patients taking glucocorticoids longer than three months, including low body mass index, parental history of hip fracture, smoking, consuming three or more alcoholic drinks a day, higher daily glucocorticoid dose, higher cumulative glucocorticoid dose, intravenous pulse glucocorticoid use, or declining central bone mineral density measurement that exceeds the least significant change.
Dr. Grossman says that the patient’s age and a history of falls are significant fracture risks. In addition to questioning all patients about recent falls, physicians should observe their patient’s gait and take an annual height measurement.
Prevention and Management
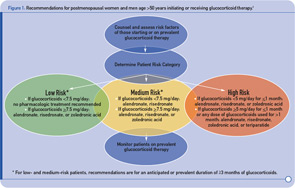
For patients who will be taking glucocorticoids for at least three months or who have taken them for three months or more already, the 2010 recommendations advise that pharmacologic treatment be prescribed for postmenopausal women and men aged 50 and older who have a low fracture risk if they are taking at least 7.5 mg or prednisone per day. This therapy can include alendronate, risedronate, or zoledronic acid. (See Figure 1)
Patients at medium or high fracture risk should begin therapy if they are taking any dose of glucocorticoids for three months or longer. Teriparatide is added to the treatment choices for patients who are at high risk. Estrogen replacement and testosterone therapies are no longer endorsed.
The recommendations are more complicated and less conclusive for premenopausal women because of the paucity of data from randomized controlled trials. “Very few of the studies had enough of a sample size to even comment on fracture outcomes in premenopausal patients,” Dr. Grossman says.
The recommendations for premenopausal women, which also pertain to men younger than age 50, only apply to those patients in that age group who have a history of fragility fracture. Pharmacologic treatment recommendations for this group are also different for a woman who has childbearing potential than for one who does not. (See Figure 2) Pharmacologic treatment, including alendronate, risedronate, or zoledronic acid, is recommended for women with nonchildbearing potential and for men in this age group if they are taking 5 mg or more of prednisone per day for one to three months. Drugs with shorter half-lives are recommended for women of childbearing potential. For any dose of glucocorticoids, if patients are on steroids or anticipate being on steroids for three or more months, the same medications and teriparatide are recommended.
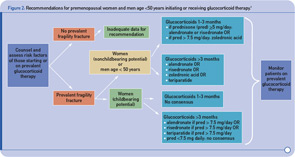
Women with childbearing potential and a history of fragility fracture who take 7.5 mg or more of prednisone per day can also be treated with alendronate, risedronate, or teriparatide. No recommendations are given for premenopausal women or men under age 50 with no history of fracture because the evidence is currently inadequate. “This is a population where a case-by-case determination needs to be made. Depending on their risk factors, bone mineral density measurements, and pregnancy plans, we may want to follow their bone mineral density more closely to see whether these studies are showing a decline if they are not on therapy,” Dr. Grossman says.
Other Preventive Strategies
All patients who begin treatment with a glucocorticoid at any dose and for any duration should be given calcium and vitamin D supplementation. Calcium intake of 1,200 to 1,500 mg per day is recommended, and vitamin D supplementation should achieve a therapeutic level of 25-hydroxyvitamin D greater than 30, or dosage of 800 to 1,000 IU per day.
“The steroids interfere with calcium absorption, so theoretically there may be reasons why patients treated with glucocorticoids should have more intake of vitamin D, but there are not a lot of data to support that,” Dr. Grossman says. “We will probably get a better idea about whether that makes a difference in fracture risk reduction as people report more data about vitamin D supplementation over the next five to 10 years.”
Many patients are unaware that they should be concerned about osteoporosis if they are taking a glucocorticoid. “Patients don’t often ask for bone density tests to be done. They wait until their doctor says they need to get one. They do, however, frequently report concerns about the negative aspects of bisphosphonates because of what is reported in the mainstream press,” Dr. Grossman says.
“I hope that patients will become more aware of the positive benefit of preventive therapy, and that they can play an important role in getting preventive care,” she continues. “If patients become aware of these recommendations and are more aware of the consequences in terms of bone health, that will improve their compliance with therapy.”
Kathy Holliman is a medical journalist based in New Jersey.

