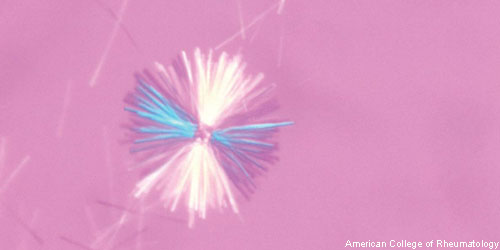
 Gout, a common form of inflammatory arthritis, results from both genetic and environmental factors. Physicians must actively manage gout patients to prevent elevated blood levels of uric acid from forming the thin, rod-like monosodium urate (MSU) crystals that deposit in the joints. These deposits lead to severe pain, stiffness and joint damage. For physicians, patient management includes considering the socioeconomic, dietary and medical factors that influence uric acid levels and/or facilitate MSU crystal formation in the patient. Such risk factors include hyperuricemia, medications, comorbidities and lead exposure.
Gout, a common form of inflammatory arthritis, results from both genetic and environmental factors. Physicians must actively manage gout patients to prevent elevated blood levels of uric acid from forming the thin, rod-like monosodium urate (MSU) crystals that deposit in the joints. These deposits lead to severe pain, stiffness and joint damage. For physicians, patient management includes considering the socioeconomic, dietary and medical factors that influence uric acid levels and/or facilitate MSU crystal formation in the patient. Such risk factors include hyperuricemia, medications, comorbidities and lead exposure.
Globally, experts estimate the prevalence of gout to be between 0.1% and 10%, with an incidence of between 0.3 to 6 cases per 1,000 person-years.1 Although the prevalence and incidence of gout vary by region, both are increasing in many developed countries.
The National Health and Nutrition Examination Survey (NHANES) evaluated the U.S. population, asking “Has a doctor ever told you that you had gout?” The survey used the answer to this question to estimate the lifetime prevalence of gout. The NHANES study found a higher age-adjusted prevalence (3.9%) from 2007–2008 than from 1988–1994 (2.9%). This significant increase in age-adjusted prevalence of gout paralleled an observed increase in hyperuricemia. However, the investigators note the NHANES prevalence values are likely an overestimate, because they are based on self-reported data. Thus, experts have called for more specific studies on the prevalence of gout in the U.S., as well as an evaluation of understudied populations that may have been missed by NHANES.2
New research presented at the Annual European Congress of Rheumatology, EULAR 2018, describes a 26.8% increase in U.S. emergency department (ED) visits for people living with gout.3 The increase occurred between 2006 and 2014. The largest increase was seen in the 45–64 years age group (28%). Gurkirpal Singh, MD, lead study investigator and adjunct clinical professor of medicine at Stanford University in Palo Alto, Calif., suggests the undermanaged of the burden of uncontrolled gout may be driving the dramatic increase in U.S. ED visits over the past nine years.
“Often, the treatment of gout focuses on alleviating the symptoms of painful gout flares. However, when escalating symptoms reach the threshold of an ED visit, this [result] suggests that the underlying accumulation of uric acid may not have been adequately addressed,” explains Dr. Singh in a press release.4
For the study, Dr. Singh and colleagues evaluated data from the Nationwide Emergency Department Samples (NEDS). Over the nine-year period, they found 1.7 million people visited EDs with a primary diagnosis of acute gout. Researchers calculated the prevalence of ED visits with a primary diagnosis of gout increased from 56.5/100,000 population in 2006 to 67/100,000 in 2014 (P<0.001). They also found men accounted for 78% of the ED visits in both 2006 and 2014.

