 ACR Convergence 2021—Although most rheumatology professionals would consider gout one of the most treatable conditions we manage, the incidence and prevalence of gout is increasing worldwide.1 Adequate diagnosis and treatment, especially in patients with cardiovascular (CV) comorbidities, remain challenging.
ACR Convergence 2021—Although most rheumatology professionals would consider gout one of the most treatable conditions we manage, the incidence and prevalence of gout is increasing worldwide.1 Adequate diagnosis and treatment, especially in patients with cardiovascular (CV) comorbidities, remain challenging.
At ACR Convergence 2021, Ralf Thiele, MD, an associate professor of medicine in the Allergy/Immunology division of the Department of Medicine, University of Rochester, New York, provided an excellent overview of available imaging modalities in gout, comparing and contrasting musculoskeletal ultrasound and dual-energy computed tomography scan (DECT). Hyon Choi, MD, DrPH, a professor of medicine at Harvard Medical School and director at the Gout and Crystal Arthropathy Center at Massachusetts General Hospital, Boston, then followed with insights into the intersection between gout and CV disease.
Gout & Imaging
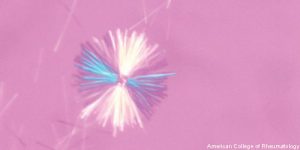
The gold standard for the diagnosis of gout remains the detection of monosodium urate crystals on synovial fluid analysis, but joint aspiration is not always a viable option, and specimen handling and interpretation may be affected by experience and training. Fortunately, advanced imaging has an evolving role in the diagnosis of gout.2
Ultrasound
Ultrasound is safe and available for bedside use, and its use in the diagnosis and management of gout continues to increase in popularity. Dr. Thiele highlighted sonographic features highly suggestive of gout: double-contour sign, tophus, aggregates (i.e., snowstorm) and erosions. Consensus-based ultrasound definitions of elementary lesions in gout have been created and demonstrate good reliability.3
The double-contour sign (i.e., an abnormal hyperechoic band of urate material overlying articular cartilage) is particularly useful because it’s sensitive to change; that is, it goes away when gout is appropriately treated.4 “Of note, calcium pyrophosphate crystals are typically found within the cartilage, but may break through and deposit over the luminal surface,” Dr. Thiele said. “Double-contour sign is typical for monosodium urate deposition in joints, but calcium pyrophosphate disease remains on the differential.”
Tophi are also appreciable on ultrasound, and power Doppler can identify hyperemia of matrix tissue associated with tophi in both symptomatic and asymptomatic patients. “Tendon insertion sites are a preferential location for tophus formation,” Dr. Thiele said. “Of note, rheumatoid nodules may appear similar on physical exam, but have a different sonographic appearance.”
Aggregates, commonly called snowstorm, are another sonographic lesion seen in gout, and the differential for these includes basic calcium phosphate crystals. “Erosions are a later gout finding,” Dr. Thiele said. “Ultrasound is slightly more sensitive for their detection than conventional radiography, and magnetic resonance imaging (MRI) typically is not specific enough for diagnosis. So ultrasound is particularly useful for detection of early gouty erosive disease,” he said.
Dual-Energy CT Scan (DECT)
Next, Dr. Thiele directed our attention toward DECT, a type of imaging that uses differences in attenuation at different energies to help differentiate calcium from urate crystals. “DECT can provide three-dimensional reconstructional imaging so you can really get an overview of where the tophi are located, but it can underestimate tophus size when compared with ultrasound,” he explained.5 “With DECT you need a certain concentration of tophaceous material per cubic space for it to be detected. So, patients with early tophaceous disease might be missed on DECT, and better appreciated with ultrasound. Ultrasound provides anatomic context and also demonstrates hyperemic inflammation, but it can miss tophi if the location is not included in the routine scanning protocol. DECT provides more of a general overview.”
Which modality should we choose? “Sensitivity and specificity are overall comparable between the two.6 So I recommend considering availability, cost, patient comfort and repeatability of imaging when deciding between ultrasound and DECT,” Dr. Thiele concluded.
Gout & CV Disease
Dr. Choi spoke next, shifting the talk toward gout and CV comorbidities. Gout prevalence continues to increase, largely driven by hyperuricemia associated with western lifestyle trends. Worsening comorbidities at the time of incident gout have increased as well, with hypertension (74%), metabolic syndrome (63%) and obesity (53%) topping the list.7 There is an independent association between serum uric acid concentration and the risk of CV disease, though causation remains unclear.
What can we do? “While the causality between urate levels, CV disease and gout remains debated and trials are ongoing, we still need to do our best to treat gout and protect our patients,” Dr. Choi said. “It would be best if we could find a medication that protected against gout and CV disease so we could reverse premature mortality trends in our gout patients.”
Recent studies have shown CV disease-protective effects from colchicine and interleukin-1 inhibition.8,9 In addition, sodium-glucose cotransporter-2 (SLGT-2) inhibitors have shown pleiotropic benefits in chronic kidney disease, and may also offer benefits relevant to gout.10 Dr. Choi hopes further studies will better elucidate how we can use medications as a “two for one.”
Dr. Choi next discussed the much-debated CV risk of xanthine oxidase inhibitors. In 2018, the CARES trial showed an increased risk of cardiac and all-cause mortality with febuxostat, resulting in an U.S. Food & Drug Administration (FDA) boxed warning for an increased risk of death.11 In 2020, data from the FAST trial contradicted those results, showing no increased risk.12
“Both trials had limitations, but the collective verdict on CV safety is that allopurinol and febuxostat are equivalent [because] the CARES trial had 45% of subjects lost to follow-up (compared with 6% in FAST), severely threatening its validity,” Dr. Choi said. Regarding febuxostat’s Boxed Warning, he noted, “I’m not sure how this will get removed. It would be ideal to incorporate the FAST trial results, in my opinion.”
Summary
In conclusion, there is still a lot to learn about the diagnosis and management of gout and the comorbidity of CV, but we are making progress. Advanced imaging is increasing diagnostic ease, and future studies may delineate drugs that address the consequences of both gout and its CV comorbidities.
 Samantha C. Shapiro, MD, is an academic rheumatologist and an affiliate faculty member of the Dell Medical School at the University of Texas at Austin. She received her training in internal medicine and rheumatology at Johns Hopkins University, Baltimore. She is also a member of the ACR Insurance Subcommittee.
Samantha C. Shapiro, MD, is an academic rheumatologist and an affiliate faculty member of the Dell Medical School at the University of Texas at Austin. She received her training in internal medicine and rheumatology at Johns Hopkins University, Baltimore. She is also a member of the ACR Insurance Subcommittee.
References
- Roddy E, Choi HK. Epidemiology of gout. Rheum Dis Clin North Am. 2014 May;40(2):155–175.
- Richette P, Doherty M, Pascual E, et al. 2018 updated European League Against Rheumatism evidence-based recommendations for the diagnosis of gout. Ann Rheum Dis. 2020 Jan;79(1):31–38.
- Gutierrez M, Schmidt WA, Thiele RG, et al. International consensus for ultrasound lesions in gout: Results of Delphi process and web-reliability exercise. Rheumatology (Oxford). 2015 Oct;54(10):1797–1805.
- Thiele RG, Schlesinger N. Ultrasonography shows disappearance of monosodium urate crystal deposition on hyaline cartilage after sustained normouricemia is achieved. Rheumatol Int. 2010;30(4):495–503.
- Desai MA, Peterson JJ, Garner HW, et al. Clinical utility of dual-energy CT for evaluation of tophaceous gout. Radiographics. 2011;31(5):1365–1375.
- Newberry SJ, FitzGerald JD, Motala A, et al. Diagnosis of gout: A systematic review in support of an American college of physicians clinical practice guideline. Ann Intern Med. 2017 Jan 3;166(1):27–36.
- Zhu Y, Pandya BJ, Choi HK. Comorbidities of gout and hyperuricemia in the US general population: NHANES 2007–2008. Am J Med. 2012 Jul;125(7):679–687.
- Ridker PM, Everett BM, Thuren T, et al. Anti-inflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017 Sep 21;377(12):1119–1131.
- Nidorf SM, Fiolet ATL, Mosterd A, et al. Colchicine in patients with chronic coronary disease. N Engl J Med. 2020 Nov 5;383(19):1838–1847.
- Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020 Oct 8;383(15):1436–1446.
- White WB, Saag KG, Becker MA, et al. Cardiovascular safety of febuxostat or allopurinol in patients with gout. N Engl J Med. 2018 Mar 29;378(13):1200–1210.
- Mackenzie IS, Ford I, Nuki G, et al. Long-term cardiovascular safety of febuxostat compared with allopurinol in patients with gout (FAST): A multicentre, prospective, randomised, open-label, non-inferiority trial. Lancet. 2020 Nov 28;396(10264):1745–1757.