In other patients, especially those with GPA, it is common to see a one-two punch, in which the patient develops eustachian tube inflammation followed by serous otitis media. They often complain of clogging like having water in the ear or the clogged effect after an airplane ride.
The first sign of chondral involvement in the nose is erythema and warmth in the distal septum. When that progresses, especially in GPA patients, it can lead to nasal septal perforation, often with copious amounts of crusting. “As it progresses, both GPA and RP patients can develop saddle nose deformity, where the bridge collapses,” said Dr. Seo.
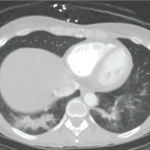
Chondritis can also affect the respiratory tract, making it too thick or too thin. “When it’s too thick, SGS [subglottic stenosis] and bronchial stenosis may result,” said Dr. Seo. “Too thin and patients develop tracheomalacia or bronchomalacia, which can lead to airway collapse.”
Some of the ocular manifestations related to RP are common, and include episcleritis/scleritis (in about 65% of cases). Dr. Seo said a broad range of ocular manifestations is associated with this diagnosis, including sicca, keratitis, optic neuritis and lid edema.
Musculoskeletal manifestations are also common. “What makes RP unique is that it can affect the sternum, so there may be involvement with the SC joints, the costochondral junctions and the sternomanubrial joints, which I think is unique for this diagnosis.”
Skin manifestations with RP are varied. They include aphthosis, purpura, livedo, urticarial, phlebitis, ulcerations and digital necrosis.
Dr. Seo said because it can be difficult to tell the difference between RP and GPA, it becomes necessary to rely on pathology to come up with a diagnosis. “For RP, that can mean seeing evidence of pleomorphic cellular infiltrate at the chondrodermal junction. Also, cartilage is gradually replaced by granulation tissue and fibrosis. For granulomatosis with polyangiitis, you may see granulomatous inflammation with multinucleated giant cells and palisading histiocytes; neutrophic, destructive angiitis; or geographic necrosis.”
Better Diagnosing May Be on the Horizon
Dr. Seo said one developing tool that may help classification in the future was presented as an abstract at the conference. (Note: Abstract No. 1719: “Clinical Phenotypes in Relapsing Polychondritis in a Prospective Cohort.”)
In the study, led by Marcela Ferrada, MD, a Lawrence Shulman Scholar at the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health, Bethesda, Md., 73 patients who meet McAdams or Damiani’s diagnostic criteria for relapsing polychondritis were selected from a prospective, observational cohort. The researchers identified three phenotypes of patients with RP that differ in time to diagnosis, clinical and radiological characteristics, and complications. They were grouped as typical (14%), airway predominant (29%) or non-destructive (57%).