The researchers concluded: “Recognizing a broader spectrum of clinical patterns of disease in RP, beyond cartilaginous involvement of the ear and upper airway, may reduce diagnostic delay and facilitate development of targeted management approaches.”
As for treatment possibilities, Dr. Seo said it’s important to remember that RP is not a single diagnosis, but has a spectrum of manifestations. “So we have to make sure the punishment fits the crime—from mild to life threatening. We must also remember that many patients can be refractory to immunosuppressive therapy and may need to be cycled through several drugs to find the right ones for them to achieve remission. It’s important to remember: You will never make a diagnosis that you are not looking for.”
When Surgery Becomes Necessary
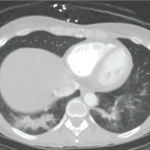
Also presenting with Dr. Seo was his colleague and collaborator, Alexander T. Hillel, MD, an associate professor in the Department of Otolaryngology, Johns Hopkins School of Medicine. The case referred to earlier in this article was that of a patient Dr. Seo and Dr. Hillel shared. After a year, the patient was ultimately diagnosed with subglottic stenosis, which had resulted in the narrowing of his trachea.
“As an otolaryngologist, I have a bit of bias toward airway involvement when it comes to RP and GPA,” said Dr. Hillel. He stressed the importance of collaboration between rheumatologists and otolaryngologists with RA and GPA patients.
He says he avoids tracheostomies when possible, as well as open surgery. “I use endoscopic procedures. As surgeons, we must make sure to not make things worse than they have to be.”
Mike Fillon is a healthcare writer living in the Atlanta area.