He was transferred to our hospital for further management of the refractory hemorrhage. A small-bowel enteroscopy revealed multiple diffuse ulcers in the third portion of the duodenum. These were thought to be the cause of the recent bleeding. The jejunal wall had adherent clots, but no active bleeding. It was hypothesized that more ulcers might have been present beyond the reach of the scope. The ulcers were clipped and biopsied. The diffuse nature of the ulcers suggested a systemic process, such as a vasculitis. The pathology report, however, described small bowel mucosa with ulceration and no evidence of granulomata or eosinophilic infiltrate.
After transfer to our facility, he had one witnessed tonic-clonic seizure episode lasting less than a minute. He was diagnosed as having posterior reversible encephalopathy syndrome and started on antiseizure medication. The third dose of rituximab was delayed due to the seizure and hypotension secondary to GI hemorrhage, but he completed a total of four doses of rituximab. The steroids were tapered according to the protocol outlined in the rituximab vs. cyclophosphamide for ANCA-associated vasculitis (RAVE) trial.2
The patient required daily blood transfusions for intestinal hemorrhage. He received aminocaproic acid in an attempt to stop the bleeding. Selective mesenteric angiography with catheterization of celiac and superior mesenteric artery was performed, but no active bleeding was visualized. An attempt to catheterize the inferior pancreaticoduodenal artery was unsuccessful.
He had severe pain and worsening abdominal distention. CT scan of the abdomen and pelvis showed a large amount of free fluid and extraluminal contrast material with pneumoperitoneum, concerning for bowel perforation. It was believed the small bowel was too diffusely involved for typical mesenteric ischemia, but thickening and edema of the small bowel were attributed to bowel vasculitis. He underwent an exploratory laparotomy with small-bowel resection and enteroenterostomy to repair the jejunal perforation.
The pathology of the resected portion showed a small transmural defect with acute serositis, consistent with perforation. Multiple ulcers were identified in the specimen.
The patient’s skin and respiratory status improved, and he was weaned off the mechanical ventilation. His renal function returned to normal. His course was complicated by the GI manifestations of his disease. Following the bowel surgery, he continued to show improvement; he was placed on tube feedings and started on an oral diet. His GI bleeding resolved completely, and he did not require further transfusions.
Discussion
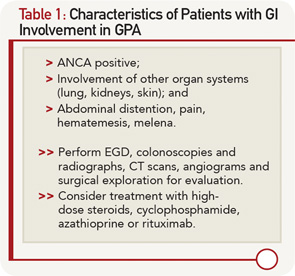
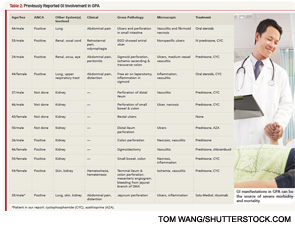
GPA affecting the GI tract has been infrequently reported in literature. There are case reports of the disease affecting parts of the digestive tract: esophagus, stomach, small intestine or colon.3 Esophagogastroscopy may reveal multiple superficial small ulcerations or small (0.5 to 1 cm) polyps in the esophagus, the stomach or the pylorus. Vasculitis mainly affects the distal small bowel or colon.