The ACR Task Force on Osteoporosis Guidelines recommend OCs to prevent glucocorticoid-induced osteoporosis in premenopausal women with oligo- or amenorrhea. However, an alternative form of contraception, medroxyprogesterone acetate injectable suspension (Depo-Provera), was associated with an increase in osteopenia/osteoporosis after two years of use in a non-SLE female population.10
Cardiovascular Considerations
While there are untoward effects of estrogens on clotting parameters, and data from the prospective Heart and Estrogen/progestin Replacement Study (HERS) and the NIH-sponsored Women’s Health Initiative have not substantiated the expected cardioprotection of hormone replacement in postmenopausal women (even suggested potential risk for coronary heart disease, albeit age from menopause is likely a factor), favorable effects of estrogens on several surrogate markers of cardiac risk may still be relevant to premenopausal women with SLE.11-13 Accumulating data on large numbers of SLE patients strongly support accelerated atherosclerosis, the precise etiology of which remains undefined. It is presently unknown whether OCs confer a beneficial cardiac effect given that estrogens increase HDL cholesterol; decrease both LDL cholesterol and lipoprotein(a); decrease circulating P-selectin, which tethers leukocytes to endothelial cells and activated platelets; and enhance basal nitric oxide production and release. Estradiol reduces the vascular response in an in vitro model of immune injury, the rabbit cardiac allograft, which may mimic the pathogenesis of SLE-accelerated atherosclerosis. Observational studies suggest that higher estrogen status is associated with a decreased mean serum total homocysteine concentration, a risk factor for vascular occlusion.14 Estrogens may have an antioxidant effect, inhibiting peroxidation of vascular smooth muscle membrane phospholipids and thereby peroxidation induced cell growth and migration, an important step in atherosclerosis.
The increased thrombotic risk associated with estrogen may outweigh its protective effects on atherosclerosis in women with established plaque, at least for the first years before longer-term cardioprotective benefits can take effect and have a major impact. Most studies suggest that estrogen inhibits the neointimal response to acute injury in normal blood vessels, but this vasoprotective effect is not seen in vessels with pre-existing atherosclerosis. In contrast, one placebo-controlled study has suggested that short term administration of 17b estradiol is effective in improving effort induced myocardial ischemia in female patients with coronary artery disease.15 Acute administration of conjugated equine estrogens prior to induction of ischemia in dogs attenuated the ventricular arrhythmias of ischemia as well as those of reperfusion.16 In nonhuman primates, OCs do not increase the risk of arterial thrombosis. In fact, there was a reduction in the incidence of thrombosis in the OC-treated animals versus untreated controls.17 Furthermore, OCs inhibited atherosclerosis in a prospective treatment study in 193 adult female cynomolgus monkeys.18
Conclusion
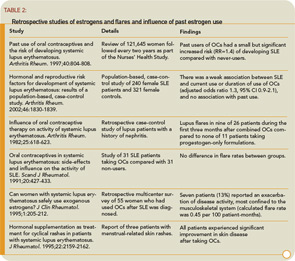
The results of three large prospective trials indicate that there is generally excellent tolerance of exogenous hormones with regard to disease activity. In contrast to the agreement of the two studies on premenopaual patients and OCs with regard to all types of flares, there was a small but significant risk of increasing the natural flare rate of lupus by adding a short course of HRT. Fortunately, the great majority of these flares were mild/moderate.


