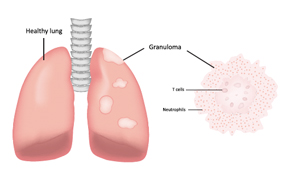
One severe life-threatening vasculitis is granulomatosis with polyangiitis.
joshya/shutterstock.com
SAN FRANCISCO—The heterogeneity of systemic vasculitis, a set of diseases characterized by inflammation of blood vessel walls, presents rheumatologists with diagnostic and treatment challenges, said Sharon A. Chung, MD, MAS, director of the University of California, San Francisco Vasculitis Clinic, at the California Rheumatology Alliance 2016 Scientific & Medical Meeting in May.

Dr. Chung
She outlined emerging therapy strategies for three types of vasculitis: giant cell arteritis, granulomatosis with polyangiitis and Churg-Strauss syndrome. Therapies under study include biological agents, such as rituximab, abatacept, tocilizumab and mepolizumab, which are being used or studied for the treatment of the other autoimmune disorders highlighted in San Francisco.
“There has been significant progress in the past 10 years in the treatment of systemic vasculitis with the advent of biologic therapies, and with multiple studies underway to help expand therapeutic options available to patients,” she said. “In the future, we hope we’ll have an expanded armamentarium of drugs for these diseases.” Meanwhile, the search continues for the holy grail of vasculitis treatment—targeted therapies that minimize toxicity and offer true steroid-sparing benefits. “In vasculitis, we are taking medications shown to be effective for other rheumatic illnesses and seeing if they can be effective for these diseases—because there might be some common pathologies,” Dr. Chung said.
GCA Preliminary Results
The current first-line therapy for giant cell arteritis (GCA) is prednisone. However, there is substantial clinical need for alternative treatments for patients who have GCA that is refractory to glucocorticoid use, cannot taper prednisone without increased disease activity, or have significant adverse effects from prednisone, Dr. Chung said. She reviewed recent studies of tocilizumab and abatacept, monoclonal antibodies now used to treat rheumatoid arthritis and other inflammatory joint diseases, in the treatment of GCA.
A Phase 2, double-blind, placebo-controlled trial from Switzerland reported in The Lancet in May, offered results that Dr. Chung called “astounding.”1 In this study, 30 patients with new-onset or relapsing GCA were randomized to receive either tocilizumab with prednisone or prednisone alone. Eighty-five percent of patients treated with tocilizumab were in complete remission at 12 weeks and at 52 weeks, compared with 40% and 20% of controls, respectively. Patients treated with tocilizumab took significantly less prednisone compared with those taking placebo. However, adverse events, including gastro-intestinal complications and eye infections, also occurred from using tocilizumab.
“This drug potentially could be first-line therapy along with prednisone for GCA, but we’re not there yet,” she said, because the results are from such a small sample. “We are awaiting results from the larger-scale GiACTA study, expected in 2018. But the prospect on the horizon is that tocilizumab could represent a long-needed complement or potential alternative to prednisone for GCA,” she said.
Identifying the efficacy of abatacept treatment for GCA is the goal of a randomized controlled trial whose preliminary results were reported at the ACR/ARHP Annual Meeting this past fall.2 Forty-one patients were randomized to receive abatacept or placebo, in addition to prednisone according to standardized taper schedule. At the end of the study, 48% of patients in the abatacept group remained relapse free compared with 31% of patients in the placebo group. “In the back of our minds, we are thinking that tocilizumab and abatacept could be used as important treatment options for refractory GCA and, potentially, could have a larger role in the initial treatment of disease,” Dr. Chung said.
GPA, Churg-Strauss Targeted in Preliminary Studies
Another severe life-threatening vasculitis is granulomatosis with polyangiitis (GPA) (previously called Wegener’s granulomatosis). There is a clinical need to identify more targeted, less toxic remission-induction therapies, as well as to find ways to optimize the use of currently approved therapies, she said. “We were hoping that rituximab, which has been approved for GPA, would be a safer medication for these patients. Unfortunately, past studies have suggested that the rate of infection for rituximab is the same as for the other remission induction therapies we use.”
A pivotal study is MAINRITSAN, which showed that rituximab was useful for maintaining remission in patients with GPA.3 However, every patient in MAINRITSAN who received rituximab received the same dose at the same frequency, Dr. Chung said. MAINRITSAN-2, currently underway, is examining whether using biomarkers to guide the frequency of administering rituximab will result in improved outcomes. Primary completion is expected for August of this year. “In many ways, rituximab has revolutionized treatment of GPA. But the question remains: What is the best way to use this medication?” she noted. “Can lab tests like ANCA or CD-19 counts tell us when to re-dose patients to maintain their remission?”
Another clinical need in GPA is for medication that can be used to treat less severe disease. “We can use cyclophosphamide or rituximab to treat life-threatening GPA, but these medications have toxicities,” said Dr. Chung. “Can we find less toxic medications to treat disease manifestations that are not life threatening?” To address this need, abatacept is being studied in the ABROGATE clinical trial for treatment of relapsing, non-severe GPA. Sixteen sites across North America are enrolling patients for this trial, including UCSF, where Dr. Chung is the site investigator.
A third vasculitis discussed by Dr. Chung is Churg-Strauss syndrome (CSS), also known as eosinophilic GPA. “There has been no therapy directly studied for remission induction or maintenance in Churg-Strauss syndrome,” she said. “Truly, there is no strong evidence supporting the use of any medication for this disease, and no true steroid-sparing effect has been documented for these patients, most of whom are steroid dependent.” Given the success of rituximab with GPA, a retrospective study of rituximab from earlier this year offers observational support for its use in CSS/EGPA.4
“What is exciting is that the first-ever large randomized trial for Churg-Strauss syndrome is underway,” investigating the role of mepolizumab, a monoclonal antibody that targets an interleukin 5, in the treatment of CSS/EGPA, she said. Past studies have offered promise for this medication in the treatment of refractory/relapsing CSS/EGPA, but the effect may not be durable after the medication is stopped, based on evidence from a single investigation, Dr. Chung noted. “If successful, mepolizumab would be the first identified targeted therapy for CSS/EGPA, which represents a major advancement in the treatment of this disease.”
Larry Beresford is an Oakland, Calif.-based freelance medical journalist.
References
- Villiger PM, Adler S, Kuchen S, et al. Tocilizumab for induction and maintenance of remission in giant cell arteritis: A Phase 2, randomised, double-blind, placebo-controlled trial. Lancet. 2016 May 7;387(10031):1921–1927.
- Langford CA, Cuthbertson D, Ytterberg SR, et al. A randomized double-blind trial of abatacept and glucocorticoids for the treatment of giant cell arteritis. Abstract 9L. 2015 American College of Rheumatology/Association of Rheumatology Health Professionals Annual Meeting: San Francisco. Date of first publication: 2015 Oct 27.
- Guillevin L, Pagnoux C, Karras A, et al. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med. 2014 Nov 6;371(19):1771–1780.
- Mohammad AJ, Hot A, Arndt F, et al. Rituximab for the treatment of eosinophilic granulomatosis with polyangiitis (Churg–Strauss). Ann Rheum Dis. 2016 Feb;75(2):396–401.


