In the past 15 years, rheumatoid arthritis (RA) has posed an economic burden on patients in Saudi Arabia due to the high cost of the medications used to treat the condition. As a rheumatology consultant, I’ve observed the economic impact on patients in one clinic in a private hospital in Riyadh.
RA is a chronic, disabling disease with negative effects on patients’ quality of life and a disproportinate economic impact on people of working age. The impact is observed in the patient’s productivity, family and society.
As rheumatologists, we follow the current recommendations from the European League Against Rheumatism (EULAR) and the ACR, which provide algorithms for the use of traditional disease-modifying anti-rheumatic drugs (DMARDs) and biologics. We choose medications guided by disease activity through physical examination, laboratory tests, radiological changes on X-rays and musculoskeletal ultrasonography.
As we all know, advances have been made in the treatment of RA, but the treatments place an economic burden on the patient, payers and society. The annual cost for an RA patient’s treatment at a private hospital can be estimated at approximately 60,000 SAR (Saudi Arabian Riyal) or ≈$15,979 yearly.
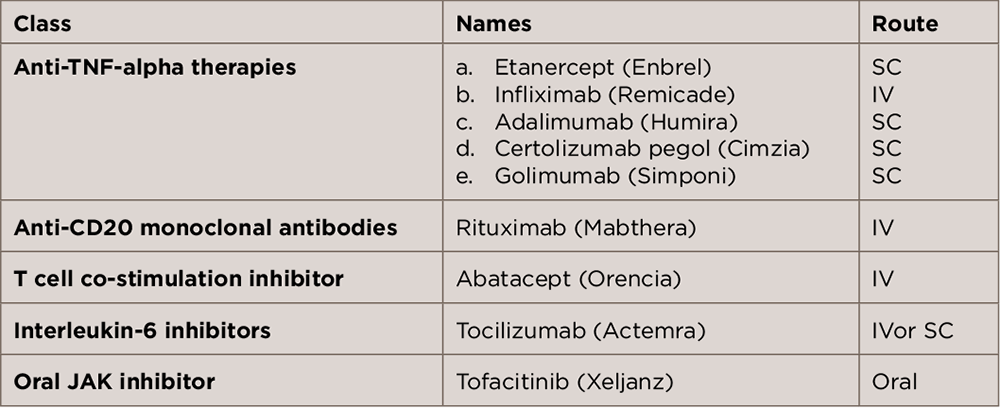
Biologic medications that we are using in our hospital are listed in Table 1 (above). The greatest impact of biologics is on the uninsured and certain insured cases. Here, I describe five different scenarios that patients in our clinic in a private hospital face to get their treatment.
Scenario 1: We all know that not all patients have the luxury of having medical insurance. Here, we call an uninsured Saudi or expatriate patient a cash patient, someone who will pay their own expenses, including purchasing at high cost their medications.
Scenario 2: Some patients have medical insurance, but their insurance refuses to pay for treatment because the disease is chronic, started before the begining date of the insurance policy or the patient didn’t indicate up front that they had the disease.
Scenario 3: The patient has insurance but the insurance company rejects the medication.
Scenario 4: At first, the patient will get approval from the insurance company and take their medication, but upon annual renewal, the insurance company will raise the cost of the insurance to the insured patient’s employer, cancel the policy or change the terms so that the insurance does not cover anything related to rheumatology.
Scenario 5: The patient is taking the medication, which has already been approved, but their employer changes its insurance company after a year, and the journey starts again.
The Way Forward
We need to help the RA patient by educating those in our surrounding environment to understand the impact of disease. We need to help patients find the best way to get the right management and to convince the insurance company to look at these cases from a different angle so that patients with ankylosing spondylitis, psoriatic arthritis and RA who are on a biologic can get the treatment they need.
In addition, we hope to find charities that can fund patients who are not insured or have problems with their insurance. Let us live 24 hours with these patients to feel their daily agony.
 Lina El Kibbi is a rheumatology consultant, adjunct assistant professor at Alfaisal University and director of medical academic affairs for the Specialized Medical Center Hospital (see image above) in Riyadh, Saudi Arabia.
Lina El Kibbi is a rheumatology consultant, adjunct assistant professor at Alfaisal University and director of medical academic affairs for the Specialized Medical Center Hospital (see image above) in Riyadh, Saudi Arabia.