Starting in 1996, new classes of antiretroviral agents became increasingly available and ushered in the era that we now know as combination antiretroviral therapy or cART (also known as highly active antiretroviral therapy or HAART). By 1997, the mortality of HIV disease had plummeted and currently has been surpassed by hepatitis C infection.2
The third phase or epoch of the HIV epidemic has progressively arisen as a result of advanced care on multiple fronts, leading to durable and perhaps lifelong viral suppression. Thus, in 2015, we rarely see treatable or untreatable opportunistic infections; however, we are formidably challenged with the sequelae of persistent immune activation. As a result, an aging HIV infected population has emerged, with an estimated one-fifth of the currently estimated 1.1 million infected U.S. patients being over the age of 55.3
Attendant to this new longevity has been the development of a number of seemingly non-AIDS-related complications, including cardiovascular disease, bone disease, sarcopenia and neurologic disease.4 These observations have led to growing concern that HIV-infected patients are experiencing premature aging and that chronic immune dysfunction, immune activation and inflammation predict and likely contribute to this excess morbidity and mortality.5,6
This concern is similar to a general concern held by practitioners who treat rheumatoid arthritis (RA); one striking area of clinical similarity between HIV infection and RA is the excess mortality from accelerated cardiovascular disease. Although the rheumatology community is well familiar with the increase in cardiovascular morbidity and mortality in RA, rheumatologists are less familiar with the similar situation with HIV.
(Click for larger image)
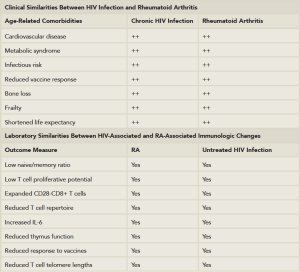
Table 1: Clinical and Laboratory Similarities Between HIV Disease & Rheumatoid Arthritis.
Adapted from: Deeks SG. HIV infection, inflammation, immunosenescence, and aging. Annu Rev Med. 2011. 62:141–155; and Weyand et al. T-cell aging in rheumatoid arthritis. Curr Opin Rheumatol. 2014 Jan; 26(1):93–100.
In HIV infection, as in RA, there is an increase of at least 50% in the relative risk for myocardial infarction when compared with well-matched controls.6,7 The relationship between these events and a persistent inflammatory state has been extensively reviewed and is not dissimilar to RA.6 Table 1 describes the potential clinical and immunologic similarities between HIV infections and RA.
Two trials demonstrate the symmetries between HIV infection and autoimmune disease: one examining the safety and effectiveness of low-dose methotrexate at reducing inflammation in adults on effective antiviral therapy and another examining the safety and potential efficacy of tocilizumab to reverse the adverse effects of persistent HIV associated immune activation in patients who have well-controlled viral infection. The future holds promise that there may be lessons learned from each field that may benefit the other.
Changing Spectrum of Rheumatic Diseases in HIV Infection in the cART Era
After the first several years of the HIV epidemic, the rheumatology community became focused on nosologically distinct rheumatic manifestations, in large part due to the seminal report by Winchester and colleagues from New York City on 13 infected individuals with severe oligoarticular arthritis with attendant features that we would now recognize as reactive arthritis.8 Because New York was among the epicenters of the epidemic, it took considerable time for rheumatologists in low-incidence areas to fully appreciate these dramatic complications.