Current State & Future Plans
The QI curriculum continues to evolve to meet the educational needs of our fellows and the clinical needs of rheumatology practice. In 2018, a second-year fellow (note: David Leverenz, now a faculty member) led the curriculum and project while concurrently enrolled in the Duke Learning Health Systems Training Program (LHSTP), which trains residents and fellows in data science methodologies that can be used to analyze health system data for clinical care, QI and research. This inspired the exploration of data streams that could be used to address one of the biggest limitations of the QI curriculum to date: the need for extensive manual chart review.
Manual chart review is universally disliked; it is tedious, time consuming and detracts from the educational value of the QI curriculum. In addition, reliance on manual chart review prevents sustainable analysis of practice patterns after each QI project concludes. For example, the 2016 project on documentation of disease-activity measures for rheumatoid arthritis required brief review of more than 3,000 patient encounters to identify more than 600 rheumatoid arthritis patient charts for detailed review. This important work led to a 38% increase in provider-documented use of RAPID3 scores in decision making; however, the only way to assess if this work led to sustainable change would be to re-do the manual chart review.
In our health system, multiple electronic health record (EHR) based tools are already available to track provider and patient data. None of these tools are perfect, and some manual data analysis will likely always be necessary for data validation. However, we have already started to realize some benefits from transitioning to these sources of data.
In 2018–19, the fellows performed a QI project focused on improving documentation efficiency. Data were collected using an EHR tool called Signal that automatically tracked metrics on provider activity within the EHR, such as documentation time and the percentage of notes composed using manual entry, dictation, smart tools and copy/paste. By using these data, fellows were able to focus on learning the principles of QI and designing PDSA cycles to improve documentation efficiency, rather than spending most of their time collecting the data.
Further, the constant stream of data allowed us to actually perform the “S” (study) part of the PDSA methodology, studying the impact of our changes in real time and using those data to inform subsequent interventions.
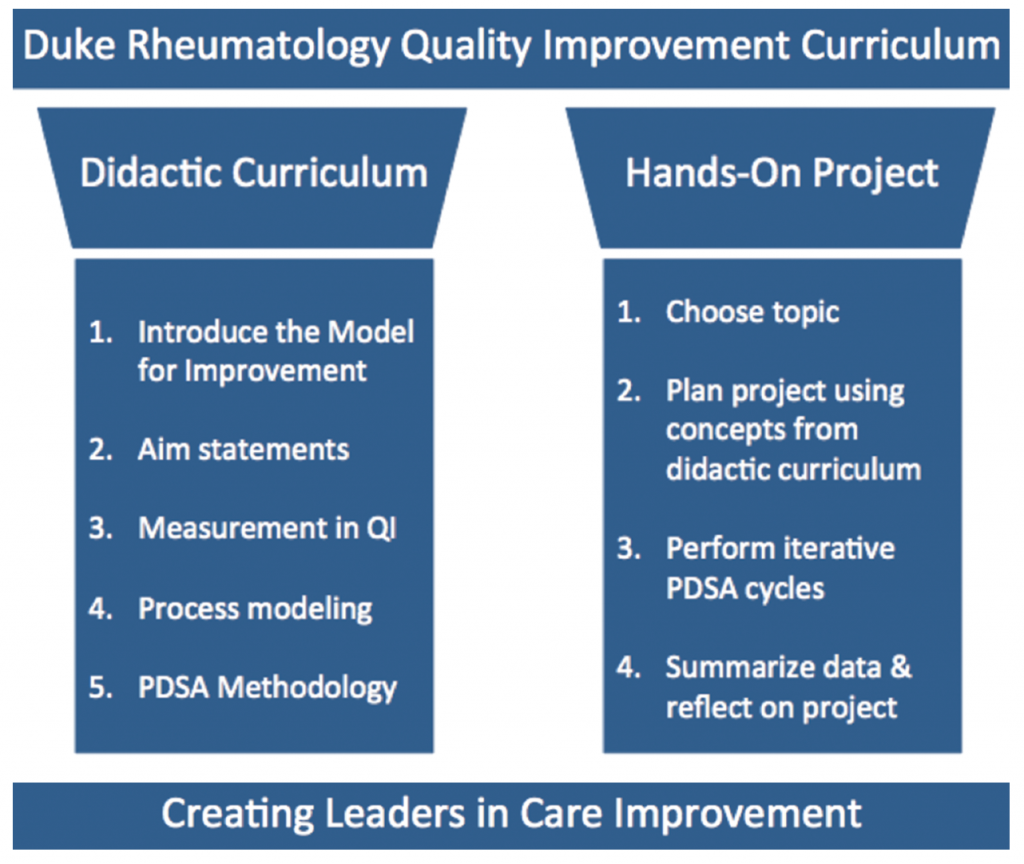
Figure 1: 2 Pillars of Success for the Duke Rheumatology Quality Improvement Curriculum
Moving forward, the objective of our QI curriculum continues to be developing rheumatologists with sufficient knowledge and experience to lead QI efforts in their future practice. This goal is balanced, but not eclipsed, by the desire to use the quality curriculum to make real improvements in our clinical practice.
Our curriculum remains based in the Institute for Healthcare Improvement (IHI) Model for Improvement, and we continue to provide a didactic series on that methodology, combined with real-world application in a yearly, fellow-led QI project (see Figure 1).
As modern medicine inches closer to the realities of value-based care, our fellows are being trained in the use of data science and learning health principles to analyze practice patterns in sustainable ways.
One doesn’t have to look far to see the value of this type of training. The RISE registry is gaining momentum, the ACR continues to develop quality measures for rheumatology practice, and legislators continue to debate the implementation of various quality incentive programs. Meanwhile, patients continue to suffer from medical errors, outdated practices, system inefficiencies, treatment delays, insufficient care and overtreatment. Upon graduation, our fellows will be ready to engage these issues and lead quality improvement initiatives for the betterment of patient care.


