A little-known committee of the American Medical Association, the Relative Value Update Committee (RUC) plays a big part in how rheumatologists and other specialists are paid, by providing recommendations that can help shape the Medicare Physician Fee Schedule (PFS). The PFS not only sets Medicare’s reimbursement rate for thousands of medical services, but also serves as the model for insurance companies in setting their own fee schedules.
Fortunately, the ACR has long had representation on the RUC, and as of this fall, one more member is joining the table: RUC trainee Luke Barré, MD, MPH, RhMSUS, a rheumatologist with Hawthorn Medical Associates in Dartmouth, Mass.
Why the RUC Matters

Dr. Barré
“I think a lot of us—myself included, until just recently—are ignorant of how important the RUC is,” Dr. Barré says. “In fact, when I first became aware of the opportunity to participate, I had to look it up to see exactly what it did.”
Through research and attendance at his first RUC meeting in September, he learned that the reimbursement decision-making process is based in large part on survey information that is reviewed and discussed by the healthcare providers on the committee. “So the only way we as rheumatologists can have any influence over those recommendations is by participating in the RUC process,” he explains.
The AMA RUC meets three times a year and advises the Centers for Medicare & Medicaid Services (CMS) about the time and effort required for various medical procedures and services to help it set appropriate reimbursement rates, explains current RUC member and rheumatologist Tim Laing, MD, MACR, associate professor emeritus at the University of Michigan Medical Center, Ann Arbor. Dr. Laing has served on the RUC for 10 years. Eileen M. Moynihan, MD, FACP, FACRH, a rheumatologist from Hadden Heights, N.J., serves as the ACR’s alternate RUC member.
Informing Value Recommendations
Because medical care is always evolving, rates for procedures or services are periodically reviewed. That review triggers the relevant professional societies, such as the ACR, to send out surveys to their members to gather information about the services in question.
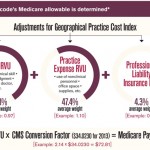
“The survey is a fairly detailed questionnaire that asks members to estimate how much effort and time go into the procedure or service under review,” Dr. Laing says. With those data in hand, the RUC has a discussion—and sometimes a lengthy debate—about whether the Relative Value Unit (RVU)for that procedure should be maintained or changed. For example, if advances in technology reduce the time or effort required to perform a service or procedure, the RUC might recommend a corresponding decrease in the RVU value.
From there, the RUC makes its value recommendations to the CMS, which usually adopts them, Dr. Laing says. “Statistically, the CMS accepts the RUC’s recommendations 80% of the time, and the other 20%, it modifies them.”
In addition, the RUC helps value new and altered codes that are assigned and defined by the AMA’s Current Procedural Terminology (CPT) committee. “For example, the CPT may split a code that it feels has become too broad in scope, perhaps because physicians have begun using a procedure in different ways to treat different groups of patients,” Dr. Laing explains. For a new procedure, the CPT would define the procedure and assign it a new code. Then those new and changed codes go to the RUC to determine their relative values.
The complexity of evaluating a wide range of specialty services highlights the need for rheumatologists to be involved. “The CMS would happily value our procedures for us,” Dr. Laing says. “But having medical societies—including the ACR— present during the discussion can ensure that the RUC has a much more accurate picture of the work that’s being done and, therefore, how it should be valued.”
Complex but Necessary
Dr. Barré attended his first RUC meeting in September, where he said the complexity of the process became apparent. “The meeting was incredibly technical and introduced me to a whole new alphabet soup of acronyms associated with healthcare funding. It felt a bit like trial by fire,” he says with a laugh. “Fortunately, my role as a trainee at that meeting was to observe and get a sense of how the RUC process works and how it influences the CMS’s incredibly important job of making decisions about the rate structure.”
That first meeting solidified his assessment that ACR representation plays a key part in how its members get reimbursed and, consequently, affects the care they can provide to their patients. It also showed why it is so crucial for ACR members to make time to fill out RUC surveys. “At the RUC, it isn’t enough for us to simply say that a particular procedure demands this amount of time and effort; we have to have surveys from our members to show it. It’s the only way that we can make a compelling argument for why we should be paid for the work that all of us do in rheumatology,” he says. “That’s why we need our members to fill out those surveys.”
The surveys are indeed critical, agrees Antanya Chung, ACR’s director of practice management. “I understand how busy rheumatology professionals are, and that this survey takes some time to fill out and can even be a bit frustrating—but it helps with the business of medicine, and the business of medicine is part of any practice,” she asserts. The ACR has videos that provide survey help, and she is also available to field questions, she adds. “The reason we so strongly encourage members to fill out the surveys is that their responses really do affect rheumatology practice today and the future of medicine overall.”
Going Forward
Although Dr. Barré realizes he still has much to learn, he is looking forward to the next meeting of the RUC where he will become a formal—albeit “very junior”—member of the ACR RUC team. He remarks, “Hopefully, I can be an effective representative of the rheumatology specialty. There is not a whole lot more important to how medicine in general, and rheumatology in particular, is practiced than how it is paid for. And the RUC is incredibly important for influencing that.”
Dr. Laing is glad to welcome a new generation of ACR participants like Dr. Barré, he says. “If we don’t have representation, we won’t have any influence over these decisions that affect our profession. Rheumatology is better served if we have a seat at the table.”
Leslie Mertz, PhD, is a freelance science journalist based in northern Michigan.