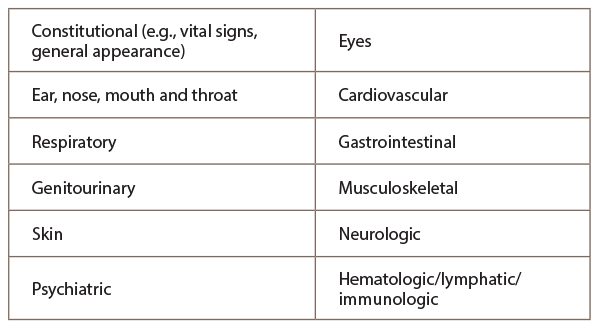
And the following organ systems are recognized:
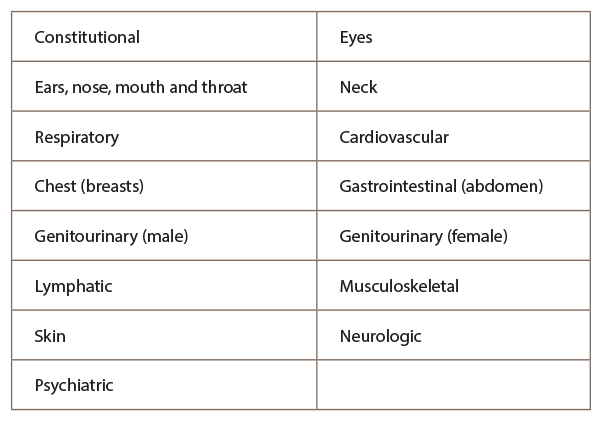
To appropriately document for the 1997 E/M examination guidelines, it’s important to note this set of physical examinations consists of the general multisystem exam or the single organ (specialty) exam, and each relies on the use of bullets from distinct organ systems:
- Problem Focused—One to five bullets from one or more organ systems.
- Expanded Problem Focused—At least six bullets from any organ systems.
- Detailed—At least two bullets from six organ systems or 12 bullets from two or more organ systems.
- Comprehensive—Two bullets from each of nine organ systems.
A comprehensive exam requires a head-to-toe examination of the ears, eyes, nose, abdomen & extremities. All exams would need to be performed & documented.
The 1997 E/M guidelines recognize the following organ systems:
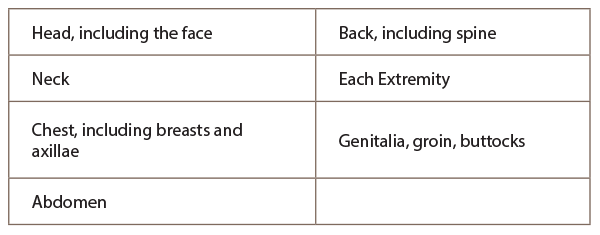
The extent of examinations performed and documented depends on the provider’s clinical judgment and the nature of the presenting problem(s). They range from limited examinations of single body areas to general multisystem or complete single organ system examinations. The Centers for Medicare & Medicaid Services (CMS) has documentation guidelines (DG) for what it wants in the patient chart(s) including, but not limited to:
- DG: Specific abnormal and relevant negative findings of the examination of the affected or symptomatic body area(s) or organ system(s) should be documented. A notation of abnormal without elaboration is insufficient.
- DG: Abnormal or unexpected findings of the examination of the unaffected or asymptomatic body area(s) or organ system(s) should be described.
- DG: A brief statement or notation indicating “negative” or “normal” is sufficient to document normal findings related to unaffected area(s) or asymptomatic organ system(s).
- DG: The medical record for a general multisystem examination should include findings about eight or more of the 12 organ systems.
The physical examination is just another component of the evaluation and management visit required to communicate among healthcare professionals evidence of patient care, as well as justifying billing for a claim. Practices are providing patients with quality care, as well as providing information documentation to ensure accurate and timely reimbursement for the services rendered to patients.
The outline provides the core pieces to document properly for the physical examination in E/M coding education. For more information on simplifying the Medicare and private payer coding guidelines to help ensure accurate reimbursement, contact the ACR coding and auditing specialists at [email protected].

