Shoulder pain is the third-leading cause for patients to seek musculoskeletal care.1,2 The impact of shoulder pain on health-related quality of life is also substantial. Shoulder pain accounted for $12 billion in direct healthcare costs in the United States in the year 2000. The etiology of shoulder pain includes rotator cuff tears, rotator cuff tendinopathy, glenohumeral arthritis, adhesive capsulitis, biceps tendonitis/tenosynovisits, acromioclavicular joint separation or degeneration, labral tears, and ligament tears. This review will differentiate the common causes of shoulder pain as well as explore the evaluation of shoulder pain by history, physical examination, and a brief overview of diagnostic testing.
History Elements
One of the most important aspects of history taking, especially relevant to rheumatology and physiatry practices, is to differentiate whether shoulder pain is the result of a primary shoulder pathology, cervical radiculopathy, a myofascial pain syndrome such as fibromyalgia or trigger points, or a systemic disorder such as polymyalgia rheumatica. The reader is likely familiar with systemic disorders leading to shoulder pain. Anecdotally, shoulder pain as a result of a primary shoulder disorder most often refers to the lateral aspect of the arm and can result in trapezial spasm when pain becomes chronic. One should suspect cervical radiculopathy if radiation is more extensive and involves the forearm and digits. This may be elicited by asking, “Does your pain travel from your neck into your shoulder (and fingers)?” A history of tingling and numbness in forearm and digits is also more commonly seen with cervical radiculopathy.
The location of pain is often not helpful in determining the etiology of shoulder pain. However, pain localized to the anterior aspect of the shoulder is often attributable to biceps tendonitis or biceps tenosynovitis. Pain localized to the superior aspect of the shoulder can be as a result of acromioclavicular joint pathology.
Once it is determined that shoulder pain is the result of a primary shoulder pathology, key history elements include whether the onset of pain was insidious and if there was an inciting event such as trauma or a fall. A fracture should almost always be ruled out in patients with a history of trauma. One has to be careful in judging whether an inciting event (as described by the patient) constitutes trauma. For instance, a patient may describe the onset of shoulder pain for the first time when they attempted to reach for an object in the backseat of a car while they were seated in the driver’s seat. Although this event may have set off a dormant rotator cuff tear, it is not a trauma/fall and has little relevance from a prognostic and/or treatment perspective. A “true” trauma includes falls, motor vehicle accidents, assault, and sports injuries. If surgery is indicated for the treatment of traumatic rotator cuff tears, an early repair is preferred to ensure optimal outcomes.3 Evidence to support this statement is, however, weak.
Other elements of history include assessment of range of motion. It is easier for patients to comprehend range of motion when assessed as limitations with a functional activity such as reaching for a jar on the top shelf (overhead activities), putting a coat on (for internal rotation), or fastening a bra in females. A history of shoulder instability or clicking suggests a labral or ligament disorder. The author recommends that physicians not familiar with instability refer their patients to a shoulder expert due to potential subtleties in the assessment, diagnosis, and treatment of such patients.
Physical Examination
As described earlier, shoulder pain can often result from a primary nonshoulder-related pathology. In such cases, it is essential to examine the involved region in addition to the shoulder. This article will only focus on musculoskeletal examination of the shoulder. In patients with suspected brachial or other proximal neuropathies, a neurological examination including sensation and reflexes is required.
Inspection: Acromioclavicular separation/deformity, dislocations, and muscle atrophy are visible on inspection of the shoulder. A bilateral comparison should be performed. Muscle atrophy can be assessed by palpation of the muscle bulk as opposed to just visual assessment. Supraspinatus, infraspinatus, and deltoid are the most commonly affected muscles. The examiner may also notice trapezial spasm (elevation of the affected shoulder) that is a common complaint in patients with shoulder disorders.
Palpation: The acromioclavicular joint and the bicipital groove are assessed for localized tenderness. If tenderness is generalized, it is less helpful in localizing the site of pathology.
Range of motion: Ideally, range of motion is measured with a goniometer. In a busy clinical setting, this is difficult to accomplish. Nonetheless, it is important to assess both active and passive range of motion. Both are reduced in adhesive capsulitis and glenohumeral osteoarthritis, whereas only active range of motion is reduced in rotator cuff tears. Range of motion should be assessed for forward flexion, isolated abduction, external and internal rotation with arm at 0º, and external and internal rotation with the arm in abduction. Detailed protocols to measure range of motion are available.4,5
Strength measurement: The author recommends measuring strength using a handheld portable dynamometer as opposed to manual muscle strength testing. Strength should be measured bilaterally for comparison. Strength measurements are performed for abduction, external rotation, and internal rotation. Detailed protocols to measure strength are available.6
Special tests: Special tests are indicated based on clinical judgment of the etiology of shoulder pain. For instance, in patients with adhesive capsulitis, no special tests are required. Moreover, it is not possible to perform special tests in such patients due to pain and limitation in range of motion. In patients with glenohumeral osteoarthritis, special tests may be difficult to perform given the limitation in range of motion but are important to assess whether the patient has a functional rotator cuff.
In patients with rotator cuff disorders, special tests are very useful. These include Neer’s sign, Hawkins sign, Jobe’s test, lag signs, bear hug test, belly press test, and Speed’s test, to name a few (see Table 1). A description of special tests can be obtained from prior reviews of the literature.6,7 The sensitivity and specificity of these tests is variable and not assessed by studies using rigorous methodology. Special tests for instability, such as O’Brien’s sign, Kim’s test, and drawer tests, also are useful to assess for labral and ligamentous pathology.8
Diagnostic Testing
Diagnostic testing for shoulder disorders may include hematology and blood chemistry, imaging tests, and neurophysiological testing. This article will focus on diagnostic imaging.
X-rays: X-rays can assist in the diagnosis of common disorders such as glenohumeral osteoarthritis. X-rays are valuable in cases of trauma where a fracture or dislocation is suspected. Degenerative changes of the acromioclavicular joint are often seen on imaging. These degenerative changes are rarely the cause of the patient’s symptoms unless the patient has localized acromioclavicular joint pain. Superior migration of the humeral head and cystic changes of the greater tuberosity are often seen in patients with rotator cuff tears due to loss of compressive forces on the humeral head.9
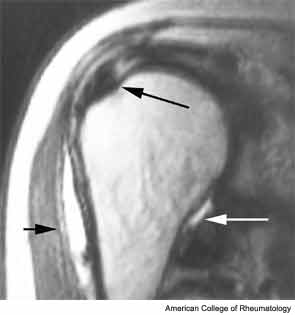
Magnetic resonance imaging (MRI): MRI is a commonly used imaging modality for assessment of shoulder pain. With the evolution of fluid sensitive sequences, MRI is very useful to diagnose rotator cuff tears, other tendon tears, and assessment of muscle. MR arthrogram is indicated for assessment of labral pathology. However, the physician has to be sensitive to costs when ordering since MRI is an expensive imaging modality. Moreover, MRI is extremely sensitive but not specific for the diagnosis of rotator cuff tears.10 In most cases, the diagnosis of rotator cuff tear can be made based on the history and physical examination findings and does not require a MRI unless surgical intervention is indicated.
Ultrasound: Musculoskeletal ultrasound has gained popularity in the last decade. The sensitivity and specificity of ultrasound for diagnosing rotator cuff tears is comparable to MRI.10,11 Ultrasound is far less expensive than MRI, can be performed in an office setting, and permits dynamic evaluation. However, ultrasound is technically challenging and user dependent.

Conclusion
In summary, a thorough history and physical examination can assist in the diagnosis of most common etiologies of shoulder pain. Imaging modalities are useful and should be reserved in cases of trauma and for surgical decision making.
Dr. Jain is assistant professor of physical medicine and rehabilitation and orthopedics at Harvard Medical School in Boston.
References
- Rekola KE, Keinanen-Kiukaanniemi S, Takala J. Use of primary health services in sparsely populated country districts by patients with musculoskeletal symptoms: Consultations with a physician. J Epidemiol Community Health. 1993;47:153-157.
- Meislin RJ, Sperling JW, Stitik TP. Persistent shoulder pain: Epidemiology, pathophysiology, and diagnosis. Am J Orthop. 2005;34:5-9.
- Pedowitz RA, Yamaguchi K, Ahmad CS, et al. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on: Optimizing the management of rotator cuff problems. J Bone Joint Surg Am. 2012;94:163-167.
- Hayes K, Walton JR, Szomor ZR, Murrell GA. Reliability of five methods for assessing shoulder range of motion. Aust J Physiother. 2001;47:289-294.
- Reinold MM, Wilk KE, Macrina LC, et al. Changes in shoulder and elbow passive range of motion after pitching in professional baseball players. Am J Sports Med. 2008;36:523-527.
- Jain NB, Wilcox R, Katz JN, Higgins LD. Clinical examination of the rotator cuff. PM&R. 2013;(In Press).
- Tennent TD, Beach WR, Meyers JF. A review of the special tests associated with shoulder examination. Part I: The rotator cuff tests. Am J Sports Med. 2003;31:154-160.
- Tennent TD, Beach WR, Meyers JF. A review of the special tests associated with shoulder examination. Part II: Laxity, instability, and superior labral anterior and posterior (SLAP) lesions. Am J Sports Med. 2003;31:301-307.
- Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990:92-96.
- Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86-A:708-716.
- Dinnes J, Loveman E, McIntyre L, Waugh N. The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: A systematic review. Health Technol Assess. 2003;7:iii, 1-166.

