As a way to gain clinical and research training in a chosen subspecialty, completing a fellowship provides young physicians with additional tools to advance their careers. To meet the growing and evolving needs of training young physicians in the specifics of a subspecialty, fellowship programs need to adapt to ever-changing educational requirements to receive the necessary accreditation and meet ongoing funding challenges.
Launching a new fellowship program can be daunting given these challenges. What are the key challenges in launching a new fellowship program in rheumatology or pediatric rheumatology? Who are the key people that need to be involved in successfully launching the program? What challenges remain going forward once a program is launched?
These were some of the questions posed to program directors of several rheumatology fellowship programs across the U.S. The programs in this article were all launched in the past several years and, therefore, offer a fresh perspective on the current requirements and challenges of developing a rheumatology fellowship program.
Funding, Funding, Funding
A key, if not the key, to launching a successful fellowship program in rheumatology or pediatric rheumatology is finding the money to support fellows. To that end, support from the Department of Medicine or hospital is crucial.
“Everyone agrees that support from the Department of Medicine is the anchor to starting a fellowship program,” says W. Neal Roberts, MD, program director of the Fellowship Program at the University of Louisville, Ky. “Their buy-in is key.”
Dr. Roberts, who is chief of the Division of Rheumatology and a professor of medicine at the University of Louisville, relaunched the university’s fellowship program in March 2013 within the larger context of revamping the entire rheumatology division. Therefore, he says initial partial funding for its fellowship program came from the university, but the funding will eventually come from the Department of Medicine as well as the local Veterans Affairs Hospital. Other monies, he says, will come from grants, endowments and clinical activities within the division.
Calling the initial funding a “recruitment startup package expense,” he says this “early phase” of funding is easy because of the support of the Department of Medicine. “But expanding beyond the initial program into a more stable program with additional faculty and fellows is a very difficult next step,” he says.
Currently, his fellowship program is a two-year program, with an option for an additional research year. One new fellow is recruited each year. With more funding, he’d like to see the program grow from one fellow the first year to two fellows the second year.
Lawrence K. Jung, MD, program director of the training program in pediatric rheumatology at Children’s National Medical Center Program, Washington, D.C., who reestablished a pediatric rheumatology fellowship in that hospital after many years of not having one, also agreed that funding is a key challenge in launching a new program. The program was approved in 2013, and the first fellow started in 2014.
Although he says the hospital is fully supportive of the program, the onus of the funding falls on his shoulders. “I need to do fundraising and look to philanthropic sources,” he says, adding that the commitment to the program by the hospital is that it will supplement the funding raised by Dr. Jung. “We are approved by ACGME [Accreditation Council for Graduate Medical Education] for two positions,” he says, “and the hospital will supplement funding for the first position.”
Funding also comes from the National Institutes of Health (NIH), which funds the last two years of the three-year fellowship program for fellows who are accepted by the NIH to spend their final two years doing research at the NIH. “If the fellow chooses not to do research with the NIH for the second and third year, then we have to come up with an alternative funding source,” says Dr. Jung, who is also chief of the Division of Rheumatology.
Support from Colleagues
Kelly A. Rouster-Stevens, MD, program director of the pediatric rheumatology training program at Emory School of Medicine, Atlanta, emphasizes the critical support needed from colleagues in completing the necessary paperwork to obtain accreditation.
“Completing the Program Information Form (PIF) was a daunting task,” she says, saying that formulating their PIF would not have been possible without the help of her colleagues.
Their program received approval from the ACGME in 2012 and had its first fellow start in July 2014, with a goal of having three fellows (one per year).
Dr. Rouster-Stevens, who is also assistant professor of pediatrics, emphasizes the critical support of a fellowship coordinator, who was instrumental in helping her learn about the internal medicine subspecialty milestones, entrustable professional activities (EPAs) and various components of maintaining accreditation. The coordinator also helps her organize fellowship applicants, arranges interviews and keeps her updated on applicants.
Dr. Roberts also emphasizes the importance of working with supportive colleagues. He says his previous experience of 15 years as program director at the Virginia Commonwealth of Virginia, where he received strong support from several people in the Department of Medicine, was instrumental in his relaunching the fellowship program in Louisville.
At the University of Louisville, he says that support came from all levels—from the deans who helped fund the division to residents who helped create the website from which prospective fellows can get needed information on the fellowship program.
One challenge for a new program, he says, is that there are no data or experience that new applicants can draw on to review the program. “Being a new fellowship program is a red flag for a fellow applicant,” he says. “The rates of fellows passing the boards over the past five years are not available, and there is no one yet leaving the program who you can ask about the strengths and defects of the program.”
He says the website helps preempt some of the questions that prospective fellows will have when considering a new program that does not yet have some of the data talked about above.
To make it even easier to address potential questions regarding its program, Dr. Roberts says that in the future the program’s website will include an FAQ section that will address potential questions in one easy-to-access format.
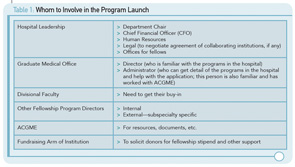
Dr. Jung also highlights the importance of a fellowship coordinator, as well as establishing relationships with internal and external sources (see Table 1).
A key, if not the key, to launching a successful fellowship program in rheumatology or pediatric rheumatology is finding the money to support fellows.
Other Challenges
Robert H. Shmerling, MD, program director of the rheumatology training program at Beth Israel Deaconess Medical Center, Boston, cites ongoing changes required for the application process as particularly challenging.
“Understanding the requirements of the ACGME during the application process and keeping up with the changes in the requirements, documentation and evaluation process are challenging,” he says. “There is no real how-to manual to consult.”
Dr. Rouster-Stevens also cites the challenge of learning the new Web-based applicant system, the Program Director’s Workstation (PDWS), as well as other systems.
“As a new fellowship director, I feel that there are too many ‘systems’ that I had to learn about with overlapping features, and I wish there was one unified system for fellowship applicants,” she says, citing PDWS, National Resident Matching Program (NRMP), Electronic Residency Application Service (ERAS), and Fellowship and Residency Electronic Interactive Database Access System (FRIEDA).
A further challenge cited by both Drs. Shmerling and Rouster-Stevens is the challenge of attracting top-notch residents to the field of rheumatology.
“Identifying outstanding fellows who are committed to a three-year fellowship including a significant research component is challenging,” says Dr. Shmerling, who is also clinical chief in the Division of Rheumatology. “Fortunately, we’ve been able to attract wonderful fellows.”
Similar to other fellowship programs, Dr. Shmerling’s program is a three-year program with two new fellows each year. The first year is devoted to clinical duties and the second two years are primarily for research, with minimal clinical duties.
Dr. Rouster-Stevens emphasizes that the low numbers of residents seeking pediatric rheumatology fellowship programs requires some advocacy to increase interest. “Our field remains one of the lowest sought after fellowship programs in terms of number of applicants compared to other subspecialties,” she says. “We need to continue to expose medical students and residents early in their training that pediatric rheumatology is a fascinating field of medicine with amazing patients, state-of-the-art research and numerous educational opportunities.”
Help from the ACR
To help program directors launch and maintain fellowship programs, the ACR offers a number of resources through tools on its website, as well as opportunities for networking and ongoing education through such venues as the recent 2014 ACR/ARHP Annual Meeting.
According to Sarah Zirkle, director of research and training, ACR, the ACR website offers a number of resources for training program directors to incorporate in their curriculum. “Graduate medical education is currently undergoing a transition into the next accreditation system, and the ACR developed a working group a year ago to develop rheumatology-specific EPAs and curricular milestones for use in rheumatology training programs,” she says, adding that the rheumatology EPAs are available now and curricular milestones will soon be available.
In addition, the ACR offers two meetings per year specifically for training directors that allow directors to discuss common issues, learn best practices and network, says Ms. Zirkle.
Funding, to help ensure a diverse and highly trained workforce is available to provide competent clinical care to those affected by rheumatic disease, is offered through the Rheumatology Research Foundation, she says. Also available through the ACR are scholarship funds to support fellows in training to attend professional meetings.
A list of educational and fellowship resources, as well as funding opportunities through grants and awards, can be found on the ACR website at http://www.rheumatology.org/Education/Training/Fellows/Information_for_Rheumatology_Fellows_in_Training.
Mary Beth Nierengarten is a freelance medical journalist based in St. Paul, Minn.
Websites of the Cited Programs
- Fellowship Program in Rheumatology, University of Louisville: http://louisville.edu/medschool/rheumatology/fellowship-program
- Fellowship Program in Pediatric Rheumatology, Children’s National Medical Center Program: http://childrensnational.org/careers-and-training/education-training/fellowships/acgme-fellowships/rheumatology
- Fellowship Program in Pediatric Rheumatology, Emory University: http://www.pediatrics.emory.edu/divisions/rheumatology/fellow/index.html
- Fellowship Program in Rheumatology at Beth Israel Deaconess Medical Center: http://www.bidmc.org/Medical-Education/Departments/Medicine/Divisions/Rheumatology/Program-Overview.aspx