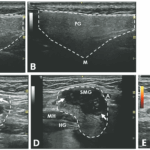
This case demonstrates a potential role of ultrasound as a diagnostic tool for evaluating salivary gland diseases. For sonographic evaluation of the salivary glands, it is important to examine both the parotid and submandibular glands, along with the thyroid gland. The parotid gland, positioned in the retromandibular fossa, exhibits an irregular wedge-shaped appearance. The submandibular gland, about half the size of the parotid gland, resides in the posterior aspect of the submandibular triangle, bordered by the body of the mandible, the anterior belly and the posterior belly of the digastric muscle. Their echotexture and homogeneity can be compared with the thyroid gland for reference.1
Various ultrasonographic scoring systems have been developed for primary Sjögren’s disease, assessing gland tissue characteristics, such as echogenicity, homogeneity, calcification, and lymph node and border clarity.2 DeVita et al. proposed a 0–4 grading scale based on hypoechoic areas, calcification and hyperechoic bands, offering a quicker and simpler approach to evaluating salivary glands.3
Ultrasound can increase sensitivity while preserving specificity for primary Sjögren’s disease beyond the 2016 ACR/EULAR classification criteria, ultimately improving overall accuracy.4 In primary Sjögren’s disease, the parotid gland is typically affected earlier than the submandibular gland. A characteristic ultrasound finding is the presence of multiple, small, oval, hypoechoic areas scattered throughout the gland, leading to an inhomogeneous appearance. These lesions resemble cysts, but lack posterior acoustic enhancement, suggesting they are dilated ducts or destroyed parenchyma filled with lymphocytic infiltrate. These lesions can also enlarge with disease progression and can exhibit increased parenchymal blood flow on color Doppler studies.1,5 However, these hypo/anechoic lesions can also be seen in amyloidosis and sarcoidosis, and there is no clear preference for parotid or submandibular gland involvement in these conditions.6
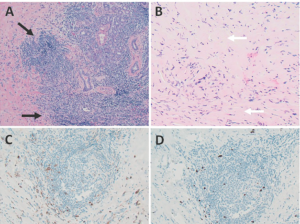
FIGURES 2 A, B, C & D: Right submandibular gland biopsy: (A) H&E staining with marked lymphoplasmacytic infiltrates (black arrows) without evidence of obliterative phlebitis; (B) fibrosis (white arrows) arranged in a swirling pattern known as storiform fibrosis, which is a hallmark feature of IgG4-RD; immunohistochemistry showed focally increased IgG+ (brown cytoplasmic
staining); (C) IgG4+ (brown cytoplasmic staining); and (D) plasma cells with a ratio of ~4:1. The key histologic features of IgG4-RD are dense lymphoplasmacytic infiltrate, storiform-patterned fibrosis, obliterative phlebitis and infiltration of IgG4+ plasma cells with ratio of
[mobile-ad name="Advert 2"]IgG4/IgG cells >40%, and >10 IgG4+ plasma cells/high-powered field in biopsy tissue sample. (Click to enlarge.)
Ultrasonography findings in IgG4-RD and Sjögren’s disease show both similarities and differences. A reticular pattern can be observed in both conditions, but a distinct nodal pattern is more common in the submandibular glands of IgG4-RD and can help distinguish it from Sjögren’s disease.7 This nodal pattern is characterized by hypoechoic, focal, homogenous areas with increased vascularity and protrusion from the surface of the glands. Submandibular glands are predominantly affected in IgG4-RD, while the involvement of parotid glands is less frequent.6 The presence of focal, hypoechoic nodular lesions primarily affecting the submandibular glands while sparing the parotid glands may indicate IgG4-RD.