BIOPHOTO ASSOCIATES / SCIENCE SOURCE
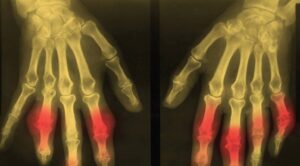
EULAR 2022 (VIRTUAL)—For years, the gold standard for gout diagnosis has been the presence of monosodium urate (MSU) crystals on synovial fluid analysis. But any practicing rheumatologist can tell you that tapping a joint isn’t always feasible. And any patient with a red, hot, swollen joint can tell you that having a needle stuck into that joint isn’t always preferable. Fortunately, imaging is becoming more and more a part of day-to-day gout diagnosis and treatment.
At the 2022 Congress of the European Alliance of Associations for Rheumatology (EULAR), Tristan Pascart, MD, PhD, full professor of rheumatology, Université Catholique de Lille, France, provided evidence-based, practical insight into the use of gout imaging modalities in clinical practice.
Diagnosis
In 2015, the ACR and EULAR published classification criteria for gout via a collaborative initiative.1 The presence of MSU crystals in a symptomatic joint, bursa or tophus was a sufficient criterion for classification as gout. If crystal analysis isn’t available, a patient could be classified as having gout via a combination of clinical, laboratory and imaging findings.
However, the criteria aren’t 100% sensitive or specific, synovial fluid analysis is invasive and often unavailable, and radiographic gout findings come too late. Additionally, Dr. Pascart noted that “clinical exam and serum urate levels don’t reflect the crystal burden in joints, which is why patients flare even after serum urate levels are at goal.”
Dual-energy computed tomography (DECT) and ultrasound are both more sensitive than plain radiographs and provide noninvasive characterization of MSU crystals with specificity. “This is why imaging findings account for half of the points you need to classify a patient as gout by the ACR/ EULAR criteria,” Dr. Pascart explained.
Ultrasound
When it comes to ultrasound, the two most important and reliable diagnostic features to look for are the double contour sign and tophi. Both are quite specific for MSU crystals. On the other hand, hyperechoic aggregates have poor inter-observer reliability and insufficient specificity.2,3 “I wouldn’t rely on aggregates alone,” Dr. Pascart cautioned.
Ultrasound is also useful as a semiquantitative tool for monitoring response to treatment. The thickness of the double contour sign can be measured over time. The double contour sign is the ultrasonographic finding that’s most sensitive to change.4
Like any test, ultrasound has its drawbacks. Dr. Pascart explained, “Ultrasound is observer dependent, and most, if not all, of the data on the diagnostic performance of ultrasound come from expert hands. So we don’t really know what happens when less expert people do it.”
