Immunology so pervades the conversations of rheumatologists that even our mindsets are determined by these antibodies and white blood cells. Our inner assumptions when we hear the word spondyloarthritis are totally different than we hear the word dsDNA. But without having reinforcement of immunological concepts, these assumptions can lead to considerable miscommunication. That’s why it’s necessary for all of us to keep reinforcing our immunological knowledge; these concepts change over time.
Speaking of change, it’s vital for practicing rheumatologists to understand the basics of clinical immunology because it forms that vital connection with basic science, clinical science and translational research. Because grant writing and publication take so much time that research is now a full-time job, there is a growing chasm between clinicians and researchers. Understanding immunology can help us narrow that chasm for the interests of our patients and advancing the field.
Anti-Boredom Antibodies
Even with these elaborated reasons, there’s a deeper justification for periodically revisiting our knowledge base regarding immunology. Immunology is fun. Immunology is full of stories that we create regarding how the world works. By listening to these stories and contributing to them, we have fun and expand the magic and joy of the world around us.
So much of what drives our burnout in clinical settings is the mundane aspect of disease. As a fellowship program director, I’ve heard trainees over the years becoming more and more bored by “another case of gout.” Certainly, we can continue our career development by just dispensing allopurinol and colchicine for gout and making our income accordingly. But without a deeper exploration into why each case of gout is unique and is a mystery worth exploring, it becomes a chore to treat the condition rather than an adventure.
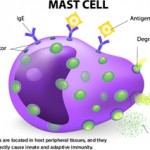
Immunology is also something that is intellectually stimulating. There’s an intangible joy that comes out of uncovering those connections between what appear to be disparate elements of the immune system. A patient of mine with chronic spontaneous urticaria developed ankylosing spondylitis. It seemed to be two separate conditions, but looking into the immunology, it appears there’s a role for mast cells in spondyloarthritis.3 Although that knowledge didn’t change the medication therapy plan, it provided me a lot of joy to connect these two dots and to relay it to a patient desperately looking for answers.
Diversity, Equity … & Immunology
The last reason it is vital for practicing rheumatologists to embrace immunology is because it has major ramifications on diversity, equity and inclusion. After all, even a cursory glance into the history of immunology shows a massive blind spot when examining the immune systems of patients from marginalized and minoritized communities.4 The clinical immunology community has been racing to identify the biases inherent within the historical dogmas of the field—and, as practicing rheumatologists, we need to be aware of these as well.