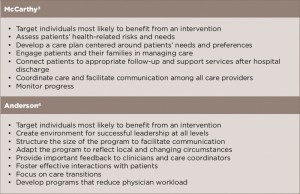
(click for larger image) Table 1: Common Features of Successful Programs to Treat High-Need, High-Cost Patients
As shown, an essential factor in both reports is correctly identifying patients who are high need and high cost and will benefit from an intervention. Also stressed are developing care plans or programs tailored to patients’ needs and circumstances, engaging patients and their families in their own care, and a focus on care coordination throughout care.
Both reports also include a list of how these key factors are implemented in a successful care program (see Tables 2 and 3, opposite). Table 2 provides a general list from the McCarthy report, and Table 3 provides a list of specific ways various programs implemented key attributes as described in the report by Dr. Anderson.
Importance of Program Design
As shown in Table 3, one of the key features for a successful program is adapting the program to reflect local and changing circumstances. This is highlighted by changes that one of the demonstration programs in the Medicare Coordinated Care Demonstration pilot undertook after initial outcomes failed to show reductions in Medicare spending and actually showed increased spending.6
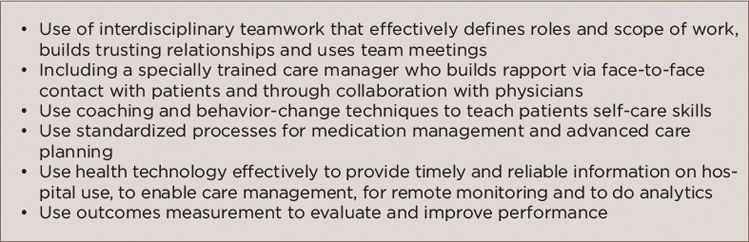
(click for larger image) Table 2: Implementation of Key Features: How It’s Done
Source: Adapted from reference No. 3.
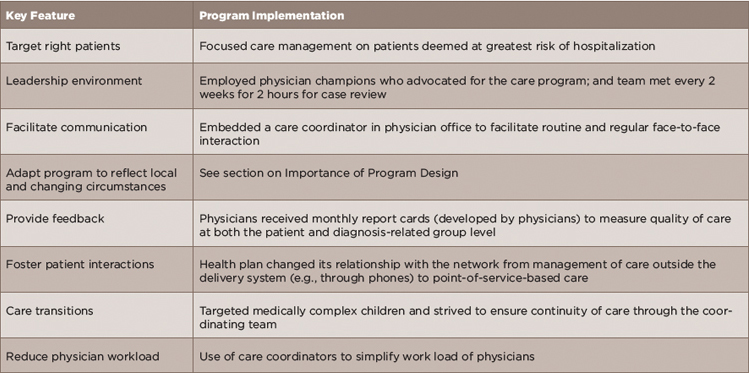
(click for larger image) Table 3: Examples of Specific Methods Used to Implement Key Features
Source: Adapted from reference No. 4.
Washington University of St. Louis School of Medicine (WUSM) was one of 15 demonstration programs selected to participate in the Medicare Coordinated Care Demonstration pilot. Mandated by the 1997 Balanced Budget Act, the Medicare Coordinated Care Demonstration pilot tested whether providing coordinated care services to Medicare beneficiaries with complex chronic conditions under the fee-for-service model could improve patient outcomes without increasing cost. Under the pilot project, participating programs received care management fees from the Centers for Medicare and Medicaid Services (CMS) in addition to Medicare payments for regular Medicare-covered Part A and B services for enrolled beneficiaries.
WUSM’s care demonstration program was initially implemented in August 2002 and ran through February 2006. Outcomes measured at that time showed that the care program did not reduce hospitalizations and in fact increased total Medicare spending by 12%.
The program was redesigned in March 2006 and included a number of changes: 1) using local care managers in St. Louis to contact (via phone and in person) all patients rather than using a remote site in California to call patients as was done in the original program design; 2) increasing in-person contacts (vs. phone contacts), especially focusing on patients considered at greatest risk of hospitalization; 3) expanding strong transitional care to all patients; 4) offering more comprehensive medication management for all patients; 5) including more thorough and systematic assessments of unmet medical and psychosocial needs; and 6) developing its own standard-of-care plans to better focus on specific conditions instead of using a care planning software program that was too broad and subjective.
