 On Nov. 4, 2022, the world lost a learned professor, a dedicated doctor, an inquisitive scientist, an adept clinician and, above all, an epitome of Athena’s representation of Mentor in Homer’s Odyssey.
On Nov. 4, 2022, the world lost a learned professor, a dedicated doctor, an inquisitive scientist, an adept clinician and, above all, an epitome of Athena’s representation of Mentor in Homer’s Odyssey.
Robert W. Lightfoot Jr., MD, had come a long way. Born in 1937, toward the end of the Great Depression, in Nashville, Tenn., he was the son of a Louisville and Nashville Railroad executive father and a supportive mother. Fast-forward to 1990, when he chaired and spearheaded the ACR’s first efforts at guideline writing, and on to 2002, when he was named an ACR Master.
Education & Career Path
Starting his education in public school, Robert showed extraordinary talent for thinking and communicating even at an early age, earning a scholarship to a prestigious private school in Nashville.
After completing his undergraduate and medical school work at Vanderbilt University, Nashville, Tenn., he headed out of state to Columbia University in New York for his intern year and second year of residency before returning to Vanderbilt for his third year of residency. He ended up back in New York the following year for his rheumatology fellowship at Columbia University. After finishing fellowship, he became an instructor in medicine at Columbia University.
In August 1966, Dr. Lightfoot enlisted in the U.S. Army Medical Corps, serving to July 1968. Upon his return from service, he passed the internal medicine board examination and followed his mentor, Charles L. Christian, MD, to the Hospital for Special Surgery, New York, where he became an assistant professor of medicine at Cornell University.
In 1972, Dr. Lightfoot sat for the inaugural rheumatology board examination. In 1976 he became chief of rheumatology at the Medical College of Wisconsin, and in 1984 he became a full professor of medicine there. He was elected to the National Lupus Hall of Fame by the American Lupus Society in 1987.
In 1987, Dr. Lightfoot moved to Kentucky to head the Division of Allergy, Immunology and Rheumatology at the University of Kentucky (UK), Lexington. Here he would settle in. It was where his children grew up, where he kept bees, took up sailing, played tennis with his wife and cared for her after she suffered a stroke.
Dr. Lightfoot served as internal medicine program director at UK from 1992 until 2003. He remained as enthusiastic about teaching as the day he became an instructor at Columbia University. After briefly retiring three separate times from UK, he returned to clinical teaching, and continued until the day before he passed away.
I [HA] had heard from my father that a professor never retires, and Dr. Lightfoot epitomized that. With his last post-retirement teaching appointment, he was told to “just write your own contract this time.”
Dr. Lightfoot’s decisions highlighted the roles of humor and family, especially after his wife, whom he loved deeply, passed away. When fellows would point out he shouldn’t be eating so many sweets, he would quip he was on a mission to raise his HbA1c, but alas he wasn’t successful. He would also slyly point out he had outlived his various primary care physicians.
He was a huge fan of college football, particularly “because the National Football League players are professionals and don’t make mistakes whilst the college players make them, which makes the game far more interesting and entertaining.” Many under his tutelage thought maybe he liked teaching for the same reason he liked college football.
In 2007 the UK rheumatology fellowship was reborn under then-Chief Leslie Crofford, MD. She hired [author] Kristine M. Lohr, MD, MS, to be program director. That brought Dr. Lightfoot and Dr. Lohr back together after 26 years. He had recruited her out of her fellowship to work at Medical College of Wisconsin. She remembers his annual pool parties at the country club. He became her model of how to be a teacher and researcher.
In 2013 Dr. Crofford returned to Nashville as professor of medicine and chief of rheumatology and immunology. Dr. Lohr became chief, and Dr. Lightfoot became her teacher again.
He had substituted Diet Coke for TaB, but not his breakfast from McDonald’s.
Teaching Philosophy
Teaching was Dr. Lightfoot’s calling, his life’s work; he would never tire of it. The saturated brains of students were the rate-limiting step in learning. While he was in New York he came across Graham R.V. Hughes, MD, FRCP, and studiously followed literature on coagulopathies, perhaps in part motivated by his own Factor V Leiden and personal experience with pulmonary emboli. Lupus erythematosus, rheumatoid arthritis and vasculitis were his other disease foci.
Most of his teaching, however—motivated by a first love—was clinical reasoning. He evolved a bedrock philosophy for this, best summarized as “Think ahead, plan ahead.” His teaching scripts were short, pointed and repeated as often as needed to create the desired effect on the learner—but not more often.
One of his pet peeves was test ordering without considering the pre-test probability. One book he would reference more than others was Beyond Normality, which deals with the likelihood of false positive results with the ever-increasing number of tests ordered, among other things.1 “An abnormal serology is not a disease,” he would reiterate.
One author [Dr. Roberts] particularly remembers Dr. Lightfoot’s critique of how patients are shunted between specialties, with no one taking responsibility for the patient. A corollary dictum that he ingrained in us was: “Never let a consult service tell you what it isn’t: Ask them what they think it is.”
He symmetrically required rheumatology consults meet the same benchmark. Fellows and colleagues were always required to tell the primary service what we thought it might be, and not just that it wasn’t rheumatologic.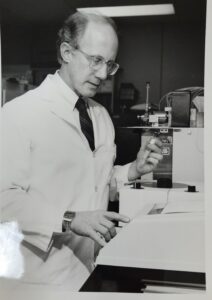
He was fond of encouraging colleagues to say, “I don’t know”—especially when the question was a prediction of a test result. When the learner had learned to say, “I don’t know,” Dr. Lightfood would reply, “I know,” perhaps drawing a quizzical look from the learner. Then it was back to clinical reasoning. He would say, “You know what the test result is going to be. It’s either positive or negative or indeterminant; what will you do in each case?”
Dr. Lightfoot also liked to remind younger colleagues that a detailed history and meticulous physical exam were also tests a physician should perform.
Follow-up appointments were also a test in this regard. He would say, “Never miss a tip from the jockey”—the jockey being the patient. “Never rush a patient” was another favorite.
As a strong proponent and practitioner of the Socratic method, he would not give answers, but rather try to chisel critical thought to help get to an answer.
He would quote Sherlock Holmes: “When you have eliminated the impossible, whatever remains, however improbable, must be the truth.” The Holmesian process then linked to his teaching script for Bayesian prior probability, the idea of placing metaphorical bets, not on patient outcomes, but on elements of the differential diagnosis and pending test results. Once the test results are back, then comes changing the bets on differential diagnoses, á la Kentucky horse racing: “You have $100 at the track. How many dollars are you going to put on your first horse?” And by horse he meant an alternative working diagnosis within the differential. Maybe that was his way of bringing Kentucky local color into didactics.
He would reiterate “plan ahead” at least once a day and would often return to the metaphorical betting analogy. “If you had $100, which horse would you bet on and how much? Why that much of your $100 on that horse and not this one?” Always have a bet, and based on new test results, findings or retaking the history, change your bet accordingly.
In treating rheumatic diseases, he championed use of the drug you know works and escalating it as fast as possible—and at the highest safe dose tolerable—to get control early, and then deescalating. With treatment options and goals, he would plan ahead and apply the decision tree model. How long will we keep a patient on a drug—especially prednisone—before evaluating whether it’s working or not? What will we do in each scenario? We need to decide that on the day we begin the medicine, so we know the agenda for the next visit.
He would advise, “Prednisone is not the real medicine. It’s what you use while you’re waiting for the real medicine to work.”
Fellows’ Thoughts
If I [HA] were to sum up his teachings in two words, those words would be “decision tree.” The last decision tree he mentioned when asked about how he felt about his hospitalization was, “Either I will die here, or I won’t.”
We weren’t prepared for the latter; Dr. Lightfoot would probably roll his eyes knowing this. He would often roll his eyes in exasperation and, sometimes, even throw his hands up with the eye roll.
Listening to the presentation of a patient after Dr. Lightfoot himself was admitted and unable to talk because he was intubated, he rolled his eyes up when told he had a borderline positive anti-nuclear antibody (ANA) with sepsis. Seeing him do that, I couldn’t help but laugh. That’s a memory I’ll cherish. Despite his predicament he could still express exasperation at the borderline ANA.
Another fellow, Kirk Jenkins, MD, noted: “I finished residency knowing—and relying on—guidelines, but he taught me how to think.
“Mentors transcend boundaries. Their teachings are not confined to one topic but rather encompass any topic you need advice on. Literally any topic—from work to home life and everything in between.
“For all of us who learned from Dr. Lightfoot, I can say with confidence that he did that. When we complained, he would say not to tell him ‘Life is hard,’ but to tell him information he could use to advise us.
“He made me [HA] a better physician, a lifelong, curious learner and a better person.
“If teaching is a science, then mentoring is an art and Dr. Lightfoot was the Bernini of mentoring. His tool was his exceptional mind, and his oeuvre the numerous minds he chiseled.”
Hammad Ali, MD, was one of the last fellows trained by Dr. Lightfoot and performed the rheumatology consult during his final illness. He is a researcher at the University of Kentucky, Lexington.
William Neal Roberts, MD, served as a junior faculty member on the ACR’s first ever guideline committee chaired by Dr. Lightfoot and shared a fellow clinic with him from 2018–22. He is a professor of rheumatology at the University of Kentucky, Lexington.
Kristine M Lohr, MD, MS, was recruited twice as a faculty member by Dr. Lightfoot, once at Medical College of Wisconsin and then again at University of Kentucky, where she ultimately served as Dr. Lightfoot’s last division chief. She is a professor of medicine and the director of the rheumatology training program at the University of Kentucky, Lexington.
Reference
- Galen RS, Gambino SR. Beyond Normality: The Predictive Value and Efficiency of Medical Diagnosis. New York: Wiley; 1978.

