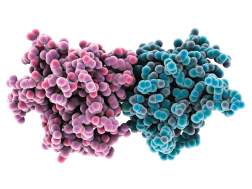
Toll-like receptor complex.
LAGUNA DESIGN / Science Source
Toll-like receptors play an important role in host defense. TLR-7 recognizes viral ssRNA, but also plays a role in the development of systemic lupus erythematosus (SLE). Genetic ablation of a similar receptor, TLR-9, results in opposite effects, with severe disease and kidney involvement. The mechanism of how this works remains unknown.
Anna-Marie Fairhurst, PhD, from the Singapore Immunology Network, and others examined how TLR-9 may suppress the development of severe SLE in a mouse model. The research was published in the October 2018 issue of Arthritis & Rheumatology.1
“It is important to understand … the role of the innate immune system in development of autoimmune diseases to devise new therapies for treating patients,” says Dr. Fairhurst. “Many innovative drugs have come from fundamental research, particularly in immunology.”
TLR-9 Deficient Mice
Dr. Fairhurst and colleagues crossed Sle1 lupus-prone mice with TLR-9-deficient mice, resulting in Sle1TLR-9-/- mice. Autoimmune disease manifestations, including kidney disease (or glomerulonephritis [GN]); autoantibody and total Ig profiles; and immune cell activation, were assessed at 4.5–6.5 months. Functional B cell studies, including Ig profiling and measuring TLR-7 expression, were completed pre-disease, at 8–10 weeks.
“Sle1TLR-9-/- mice were compared with the Sle1 mild autoimmune-prone strain,” says Dr. Fairhurst. “These mice develop antibodies, but not kidney disease.”
Sle1TLR-9-/- mice developed severe disease similar to that seen in TLR-9 deficient MRL and Nba2 models. They presented with splenomegaly due to an expansion of all major leukocyte subsets. Increases in CD138+B220- plasma cell numbers and decreases in the frequency of marginal zone B cells were observed. These are characteristics of lupus models overexpressing TLR-7. CD4+ and CD8+ T cells had a more activated phenotype in Sle1TLR-9-/- mice.
Pathological examination showed the majority of Sle1TLR-9-/- mice had class III-IV GN characterized by segmental to global endocapillary proliferation of the glomeruli. This was confirmed by increased serum BUN and urinary proteins.

Dr. Fairhurst
TLR-9 deficiency in Sle1 mice skews the autoantibody profile toward RNA-associated antigens. Further analysis using a HEp-2 cell assay showed serum antibodies in Sle1TLR-9-/- mice bound mostly to cytoplasm with some nucleolar specificity. All Sle1TLR-9-/- mouse sera lost the ability to bind mitotic chromatin.
In contrast, Sle1 mouse antibodies were binding to the nucleus. The cytoplasmic HEp-2 staining pattern of Sle1TLR9-/- serum was similar to RNA-
reactive autoantibodies. Multiplex assays of immunoglobulin (Ig) levels indicated TLR-9 deficiency resulted in higher concentrations of IgG2a/c, IgG2b and IgM autoantibodies compared to Sle1 controls.
Analysis of intracellular TLR-7 protein showed a systemic increase in expression in Sle1TLR-9-/- mice. TLR-7 levels were significantly higher in B cells, pDCs, CD11b+ DCs, macrophages and in CD11c+MHCII-precursors compared with Sle1 controls.