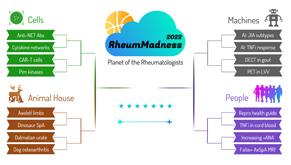
 Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The more your picks match those of our Blue Ribbon Panel of rheumatologists, the more points you get. Learn more about the panel and how the brackets work online.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn more on the RheumMadness website.
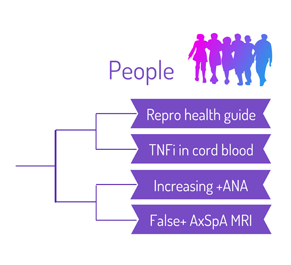
Region: People Team: False Positive MRI in Axial SpA
Classification criteria exist to homogenize patients for clinical trials. In practice, however, we often lean on them as diagnostic tools—especially when the diagnosis is unclear, which happens often in the field of rheumatology, much to the disdain of many residents and students.
 Several classification criteria for spondyloarthropathy (SpA) exist, and two are discussed most commonly: the Assessment of SpondyloArthritis International Society criteria (ASAS) and the modified New York criteria (mNY).1,2 The latter provide a very high specificity for SpA. However, as kind rheumatologists who want to treat patients before significant disease develops, we often reach for the imaging arm of the ASAS criteria to identify patients with non-radiographic axial SpA (nr-axSpA).
Several classification criteria for spondyloarthropathy (SpA) exist, and two are discussed most commonly: the Assessment of SpondyloArthritis International Society criteria (ASAS) and the modified New York criteria (mNY).1,2 The latter provide a very high specificity for SpA. However, as kind rheumatologists who want to treat patients before significant disease develops, we often reach for the imaging arm of the ASAS criteria to identify patients with non-radiographic axial SpA (nr-axSpA).
Our base article challenges the current definition of nr-axSpA. In this study, magnetic resonance imaging (MRI) findings of 793 German volunteers from the general population were examined. Positive findings were defined as the presence of bone marrow edema in sacroiliac (SI) joints, bone marrow edema in the vertebral column or fatty lesions in the vertebral column in two or more consecutive slices, in accordance with the ASAS definition.3
Researchers found bone marrow edema in SI joints in 17.2% of study participants, bone marrow edema in the spine was present in 27.5% of subjects and vertebral column fatty lesions were evident in more than 80% of subjects.
Although participants were not asked about inflammatory back pain symptoms, the number of positive MRI findings in this study drastically exceeds the expected prevalence of SpA in Germany, which is estimated to be 1–1.4%.4 When Berlin scores—a tool quantifying the degree of edema in SI joint and vertebral column—were used, the median scores were low.5 The authors say this finding is in line with research showing deep bone marrow edema ≥1 cm is strongly associated with axSpA.
No correlation exists between MRI findings and HLA-B27 positivity or the presence or duration of chronic back pain. Findings in the spine were more prevalent with increasing age, leading the authors to suggest degenerative changes were likely picked up on the MRIs.
Implications
The base article raises several questions. First, how important is it to detect nr-axSpA early? One study showed the progression from nr-axSpA to ankylosing spondylitis (AS)—meeting mNY imaging criteria—of 12% over two years with elevated C-reactive protein (CRP) level being the best predictor of progression.6
Another paper demonstrated that 50% of patients who initially met mNY criteria were reclassified as mNY-negative at their five-year follow-up, and 5% of nr-axSpA patients progressed to mNY-positive status.7 Thus, progression to AS appears slow, and even patients initially diagnosed with radiographic disease may have transient or subtle changes that are later deemed normal.
The next question: Does treating patients with nr-axSpA early improve outcomes? One randomized, controlled trial examined 80 patients with negative SI joint X-ray and inflammatory back pain, ≥2 SpA features and high Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) scores and found no difference between etanercept and placebo treatment after six months.8
Another trial (ABILITY-1) showed adalimumab was more effective in patients with nr-axSpA, with either positive CRP or sacroiliitis at 12 weeks. Most patients were also HLA-B27 positive.9
So what else can cause bone marrow edema? It’s well described in professional athletes, non-athletes exercising more aggressively (be careful with your New Year’s resolutions, y’all) and even post-partum women.10,11 Further, sarcoidosis, diffuse idiopathic skeletal hyperostosis, hyperparathyroidism, osteitis condensans ilii, Paget disease and infectious arthritis can mimic or cause sacroiliitis appearance on imaging and be wrongly diagnosed as SpA.11–14 Transient changes in SI joint are also detected in some reactive arthritis patients but require no treatment.12
Overdiagnosis of SpA can lead to missing other diagnoses, psychologic stress to patients, risk of litigation and high cost to patients and society.14 To address these issues, a new trial by Spondyloarthritis Research and Treatment Network (SPARTAN), called Classification of Axial Spondyloarthritis Inception Cohort (CLASSIC), aims to validate ASAS criteria with a more stringent definition of inflammation on MRI and independent review of all imaging studies with a five-year follow-up to be completed in 2024.15 To be discussed in RheumMadness 2025.
Chances in the Tournament
We think our team fares quite well in our region and the tournament overall. As rheumatologists, we are all painfully aware of how difficult the diagnosis of SpA can be, and we may become distracted by the other teams in the tournament with potentially excellent stats. There are animals sadly having human diseases, molecular biology galore and—the topic of every rheumatologist’s favorite consult—Increasing +ANA.
Our team’s base article challenges the instinct to lean on fancy enhancers, such as shiny MRIs/DECTs/PETs, and reminds us that a good history and a detailed physical exam performed by a caring human remain the real MVPs of rheumatology.
Anastasiya (Stacy) Bagrova, MD, is a first-year rheumatology fellow in the University of South Florida Rheumatology Fellowship Program, Tampa.
Shreya Gor, MD, is a second-year rheumatology fellow in the University of South Florida Rheumatology Fellowship Program, Tampa.
Joanne Valeriano-Marcet, MD, is program director of the University of South Florida Rheumatology Fellowship Program, Tampa.
Larry Young, MD, is chief of the Rheumatology Division at James A. Haley Veteran’s Hospital, Tampa.
John Carter, MD, is chair of the Division of Rheumatology at the University of South Florida, Tampa.
References
- Linden SVD, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. Arthritis Rheum. 1984 Apr;27(4):361–368.
- Rudwaleit M, van der Heijde D, Landewé R, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): Validation and final selection. Ann Rheum Dis. 2009 Jun;68(6):777–783.
- Baraliakos X, Richter A, Feldmann D, et al. Frequency of MRI changes suggestive of axial spondyloarthritis in the axial skeleton in a large population-based cohort of individuals aged <45 years. Ann Rheum Dis. 2020 Feb;79(2):186–192.
- Braun J, Schwarting A, Hammel L, et al. Medical care situation of patients with ankylosing spondylitis and psoriatic arthritis in Germany: Medical care situation of patients with spondyloarthritis (SpA): Ankylosing spondylitis (AS) and psoriatic arthritis (PsA) from the perspective of rheumatologists in private practice and hospitals in Germany-Results of the research project “SpA Loop-Life of Outpatients.” Z Rheumatol. 2019 May;78(4):372–381.
- Carmona L, Sellas A, Rodríguez-Lozano C, et al. Scoring with the Berlin MRI method for assessment of spinal inflammatory activity in patients with ankylosing spondylitis: A calibration exercise among rheumatologists. Clin Exp Rheumatol. Nov–Dec 2013;31(6):883–888.
- Poddubnyy D, Rudwaleit M, Haibel H, et al. Rates and predictors of radiographic sacroiliitis progression over 2 years in patients with axial spondyloarthritis. Ann Rheum Dis. 2011 Aug;70(8):1369–74.
- Sepriano A, Rudwaleit M, Sieper J, et al. Five-year follow-up of radiographic sacroiliitis: Progression as well as improvement? Ann Rheum Dis. 2016 Jun;75(6):1262–1263.
- Rusman T, van der Weijden MA, Nurmohamed MT, et al. Is treatment in patients with suspected nonradiographic axial spondyloarthritis effective? Six‐month results of a placebo‐controlled trial. Arthritis Rheumatol. 2021 May;73(5):806–815.
- Sieper J, van der Heijde D, Dougados M, et al. Efficacy and safety of adalimumab in patients with non-radiographic axial spondyloarthritis: Results of a randomised placebo-controlled trial (ABILITY-1). Ann Rheum Dis. 2013 Jun;72(6):815–822.
- Tarantino U, Greggi C, Cariati I, et al. Reviewing bone marrow edema in athletes: A difficult diagnostic and clinical approach. Medicina (Kaunas). 2021 Oct 22;57(11):1143.
- de Winter J, de Hooge M, van de Sande M, et al. Magnetic resonance imaging of the sacroiliac joints indicating sacroiliitis according to the Assessment of SpondyloArthritis International Society definition in healthy individuals, runners, and women with postpartum back pain. Arthritis Rheumatol. 2018 Jul;70(7):1042–1048.
- Robinson PC, van der Linden S, Khan MA, et al. Axial spondyloarthritis: Concept, construct, classification and implications for therapy. Nat Rev Rheumatol. 2021 Feb;17(2):109–118.
- Uslu S. Sacroiliitis in sarcoidosis mimicking ankylosing spondylitis. Rheumatology (Oxford). 2021 Feb 1;60(2):991–992.
- Antonelli MJ, Magrey M. Sacroiliitis mimics: A case report and review of the literature. BMC Musculoskelet Disord. 2017 Apr 22;18(1):170.
- Berthelot JM, Le Goff B, Maugars Y. Overdiagnosing early spondyloarthritis: What are the risks? Joint Bone Spine. 2013 Oct;80(5):446–448.
- Classification of axial spondyloarthritis inception cohort (CLASSIC). Spondyloarthritis Research and Treatment Network (SPARTAN). 2022.
 Experience All of RheumMadness
Experience All of RheumMadness
During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports. Check out the reports from each region:
Region: Cells
Region: Animal House
Region: Machines
Region: People
• False Positive MRI in Axial SpA
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The winner of each match-up is decided by a seven-member Blue Ribbon Panel of rheumatologists. The panel will vote based on which topic they think is most important to patients, providers and researchers—both now and in the future. The more your picks match those of the panel, the more points you get. The tournament results will be released in four rounds from March 26–April 4. Prizes will be given to participants with the top scores in the following categories: 1) attending/APP, 2) fellow and 3) resident/medical student. The prize is a custom RheumMadness coffee mug and a lifetime of bragging rights.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn on the RheumMadness website.


