
Rheumatologists are careful historians. They listen attentively to their patients, scouring their histories for clues that might lead to the correct diagnosis. They are always on the hunt for tangible evidence of an inflammatory process, because many of the diseases they treat are characterized by a litany of subjective complaints and a paucity of physical findings. Among the most worrisome words they may hear in the patient’s history or observe firsthand in their exam is the f word. No, not that one! I am referring to fever.
The presence of fever sounds an alarm, alerting caregivers to the possibility of infection and its dire consequences if the source and site are not quickly identified and treated appropriately. However, to rheumatologists, fever does not always connote infection. Clinical experience and recent research evidence have identified fever as a danger signal, apprising our brain and our immune system to excessive cytokine activation, whether due to infection or molecular mutations in the innate immune system.
Although fever is triggered by the stimulation of the thermoregulatory neurons nestled in the housekeeping hub at the base of our brains, better known as the hypothalamus, the cytokines that are critical for raising core temperature were only recently elucidated. Our colleague, Charles Dinarello, MD, professor of medicine at the University of Colorado in Denver, was the first investigator to observe that leukocyte pyrogen, a fever-inducing protein derived from white blood cells, alerted the hypothalamus to the danger lurking somewhere in the periphery.1
Around the time of this seminal observation, I was a medical resident involved in the care of a patient whose febrile illness highlighted the perils of failing to promptly identify a fever’s inflammatory origins. Monique was a 22-year-old student who celebrated her graduation from college by taking an extended backpacking trip through Central America. She hiked for miles through muddy rain forests and trekked along many treacherous mountain trails. When she finally returned to Montreal sometime in the dead of winter (which, in Montreal, can be just about any month except July!), she developed a fever. At first, she ignored the prickly warm sensation coursing through her body, assuming it would soon pass. But after several days of spiking temperatures to 105°F, she found herself drenched in sweat, lying in a hospital bed.
Given her recent travel to Central America, the medical team focused on a laundry list of potential infectious possibilities. These included tropical diseases rarely seen north of the 49th parallel: Chagas disease, dengue fever, yellow fever, typhoid fever, malaria and mycobacterial infection. Myriad tissue and fluid cultures failed to provide any solid clues.
Monique’s fevers blasted through multiple courses of antibiotics that were prescribed empirically. We had just two laboratory clues to work with: a marked leukocytosis and repeatedly elevated liver enzymes.
About 10 days following her admission, we were provided with a third clue, a pain in her groin. Monique had trouble walking to the bathroom, and she winced when we tried to flex or rotate her right hip. In those prehistoric days prior to the advent of magnetic resonance imaging or computed tomography, advanced hip imaging consisted of simple dye-contrast X-ray arthrography. We were astonished when the surprisingly crisp silhouette images confirmed that the typically smooth articular surface of a 22-year-old femoral head had been irreparably damaged. All in a matter of a few weeks.
A needle biopsy of the hip joint yielded inflamed, but sterile, synovial tissue and fluid. We were frustrated. How could a microbe resist an impressive array of antibiotics, destroy Monique’s hip and not leave a trace of its identity behind?
Our team was running out of ideas. Then, one afternoon, as we hovered over her bedside, someone spotted a faint salmon-colored rash spreading over Monique’s torso. It seemed to coincide with her fever spike, which occurred around 5 p.m. on most days. Suddenly, everything seemed to fit. The quotidian fever spike, the faint rash, the sterile monoarthritis, the abnormal lab results and the negative microbial cultures. We now knew the truth. Monique’s fever was merely a red herring. Just as the pungent odor of this fish was used to mislead the scent hounds on a hunt, so too, did her high fever throw all of her doctors off course. We were all focused on the likely diagnosis of an infection, but in reality, her illness had little to do with microbes and more to do with how the body can mistakenly activate aberrant pathways of inflammation.
Adults Behaving Like Children
Until the 1970s, the illness named for the British physician Dr. George Still was considered to be a disease of childhood. Looking back, it’s apparent that isolated adult cases of Still’s disease had sporadically been described in some published series of patients with fevers of unknown origin.2 In parts of Europe, the condition was known as subsepsis allergica or Wissler-Fanconi syndrome. The term adult Still’s disease was first used by the eminent British rheumatologist, Eric Bywaters, MB BCh, of the Royal Postgraduate Medical School in London, England, to describe a series of 14 adult patients seen over the course of several decades.3 Whether in young children or adults, it is the quotidian spiking fever, usually peaking in the late afternoon or evening, that distinguishes Still’s disease. The absence of any significant articular complaints in some patients may mislead treating physicians. As Dr. Still presciently described:4
The pyrexial periods are not usually associated with any clinically demonstrable exacerbation of the joint trouble, nor indeed is it possible to usually find any definite cause of the fever.
In our case, it was just the opposite; Monique’s destructive hip monoarthritis along with her fever implied infection.
A fever in a rheumatology patient can have a chilling effect on the treating clinician. On the one hand, we are compelled to assume the likelihood of an underlying infection. Although an exhaustive series of tests may fail to yield a culprit, confirming a negative result can be a daunting task.
Defining a Fever
Until the dawn of the golden age of microbiology, the era of Koch and Pasteur, clinicians usually considered fever to be a final diagnosis rather than a symptom of a disease. Documenting a fever was challenging enough due to the lack of instruments, such as thermometers that could measure body temperature. Carl Wunderlich, MD, of Leipzig University in Germany is credited as being among the first clinicians to quantify fever in patients. During the mid-19th century, using a cumbersome device that measured 1 foot long and took 20 minutes to measure a temperature, he painstakingly recorded more than 1 million readings by pressing this device into the axillae of 25,000 patients. He concluded that temperatures above 38.0°C (100.4°F) should be considered a fever.5
A Fever in The Brain
Now that body temperature could be measured accurately, investigators began to focus on the pathophysiology of fever. This puzzle was not easily unraveled; in fact, there still remain several unanswered questions. What is known suggests that the generation of a fever requires the coordinated activities of several key components of our immune system.
Circulating pyrogenic cytokines, such as interleukin (IL) 1, tumor necrosis factor (TNF) alpha and IL-6, alert the hypothalamus to danger in the periphery. Receptors for these cytokines that are present on the surfaces of brain microglial cells activate the arachidonic acid pathways, causing the release of prostaglandin E2 (PGE2). The PGE2 then acts on neurons in the preoptic area of the hypothalamus, which respond by regulating temperature. These neurons are also connected to neural pathways that regulate sleep and eating. This helps to explain, in part, why fever is associated with somnolence and loss of appetite.6 Recently, using a murine model, researchers identified RANKL/RANK as a critical element in the mediation of gender-specific, physiological thermoregulation.7 The authors speculate this pathway may be critical for the generation of menopause-associated hot flashes in some women.
Lucky 7
With the subsequent availability of antibiotics, clinicians were able to successfully eradicate the causes of most fevers. However, it became evident that a sizeable percentage of patients with persistent fevers did not have an infectious cause. This observation was borne out by the classic study of unexplained fevers by Paul Beeson, MD, and Robert Petersdorf, MD, both professors of medicine at the University of Washington in Seattle.8 They proposed three broad explanations for a persistent fever, namely infection, cancer and what they referred to as the collagen diseases. All told, diseases within the purview of rheumatology accounted for nearly one-third of the patients in their study. This diverse group included patients with rheumatic fever, systemic lupus erythematosus, cranial arteritis, sarcoidosis, nonspecific pericarditis and what was referred to as periodic disease.
The periodic fever syndromes constituted a curious group: They were poorly understood and rarely seen or described in the literature. Working at the American University in Beirut, Lebanon, Hobart Reimann, MD, professor of medicine at Jefferson Medical College in Philadelphia, had suggested the term periodic disease to describe a group of disorders “of unknown origin [that] often begin in infancy, recur uniformly at predictable times for decades without affecting the general health and resist treatment.”8 But this characterization was greeted with considerable skepticism. Perhaps this related to Reimann’s emphasis on the need for the febrile cycles of fever to last for seven days or some multiple of the number seven. In his words, “Seven always has had a special significance and looms large in folklore some cosmic association may be suspected.”8 Enough said!
One explanation for the unusual geographical distribution of BD is that a genetic risk factor may have been propagated through previously isolated communities by itinerant traders or earlier pastoral nomads whose path across Asia was determined by the natural geographic features of the continents.
Horror Autoinflammaticus
Nearly a half-century later, a series of breakthrough discoveries made in London, England, laid the groundwork for our understanding of how immune regulation intersects with the febrile response. Using cells derived from family members afflicted by the TNFR1-periodic syndromes or TRAPS, the investigators described in elegant molecular detail, the germline mutations in the TNF receptor (TNFR1) that led to the development of this dominantly inherited syndrome of fever and widespread inflammation.
Around the same time, two groups of investigators, one multinational and the other based in France, independently identified the gene responsible for another periodic disease, familial Mediterranean fever (FMF). Because TRAPS and FMF are characterized by seemingly unprovoked, recurrent episodes of fever, serositis, arthritis and cutaneous inflammation, it was not a far-fetched idea to consider that these disorders might serve as prototypes for an emerging family of inflammatory diseases.9 The term autoinflammation was coined to distinguish these unique diseases from the more commonly observed autoimmune disorders. The key distinction between these two groups is the reliance of the former group on the phylogenetically ancient, hardwired, rapid-response innate immune system; whereas the latter group relies on the more plastic, adaptive immune system.
In addition to the spectrum of periodic fever syndromes, the autoinflammatory diseases cast a wide net and include granulomatous disorders, such as sarcoidosis and Blau syndrome; storage diseases, such as Gaucher’s; Behçet’s disease; the crystalline arthropathies, such as gout and pseudogout; and adult Still’s disease, to name a few. In the course of just a decade, such terms as inflammasome, cryoprin and danger signals have become commonplace in the rheumatologist’s vocabulary.
Following The Silk Road
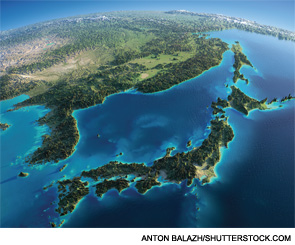
For years, clinicians have been intrigued by the curious geographic distribution of Behçet’s disease (BD). Its highest prevalence occurs across Asia in countries between 30° and 45° latitude north, where the disease runs a more severe course than in other parts of the world.10 One explanation for the unusual geographical distribution of BD is that a genetic risk factor may have been propagated through previously isolated communities by itinerant traders or earlier pastoral nomads whose path across Asia was determined by the natural geographic features of the continents. The most likely path they traveled would have been the Silk Road.
Silk was a highly valuable commodity. It was a key product in the Chinese economy, and controlling its availability made silk a valuable tool of China’s foreign policy. The traditional founder of the Silk Road is considered Zhang Qian, a courtier dispatched westward in 121 BC to bring back the unusually powerful horses, which roamed in present-day Uzbekistan. A trail heading westward from China was started, and over the centuries, traders extended it all the way to the Mediterranean Sea.10
Whenever I think of the Silk Road, I recall my patient Monique. I saw her for the last time about a year following her total hip replacement surgery. She was feeling well. Her hectic fevers had resolved. She told me that she still had the travel bug and was hoping to visit China and Tibet one day. I wonder if she ever took that trip.

Simon M. Helfgott, MD, is associate professor of medicine in the division of rheumatology, immunology and allergy at Harvard Medical School in Boston.
Note (10/19/2014): In the editorial above, I should have credited the seminal research of Daniel Kastner MD, PhD, senior investigator, Metabolic, Cardiovascular and Inflammatory Disease Genomics Branch, and head, Inflammatory Disease Section, whose numerous scientific contributions established the field of autoinflammatory disease, a term he coined.
References
- Dinarello CA, Wolff SM. Molecular basis of fever in humans. Am J Med. 1982 May;72(5):799–819.
- Larson EB. Adult Still’s disease. Evolution of a clinical syndrome and diagnosis, treatment and follow-up of 17 patients. Medicine (Baltimore). 1984 Mar;63(2):82–91.
- Bywaters EG. Still’s disease in the adult. Ann Rheum Dis. 1971;30(2):121–133.
- Still GF. On a form of chronic joint disease in children. Med Chir Trans. 1897;80:47–60.9.
- Mackowiak, PA, Wasserman SS, Levine MM. A critical appraisal of 98.6°F, the upper limit of the normal body temperature, and other legacies of Carl Reinhold August Wunderlich. JAMA. 1992 Sep 23–30;268(12):1578–1580.
- Steinman L. Nuanced roles of cytokines in three major human brain disorders. J Clin Invest. 2008 Nov;118(11):3557–3563.
- Hanada R, Leibbrandt A, Hanada T, et al. Central control of fever and female body temperature by RANKL/RANK. Nature. 2009 Nov 26;462(7272):505–509.
- Petersdorf RG, Beeson PB. Fever of unexplained origin: Report on 100 cases. Medicine (Baltimore). 1961 Feb;40:1–30.
- Masters SL, Simon A, Aksentijevich I, et al. Horror autoinflammaticus: The molecular pathophysiology of autoinflammatory disease. Annu Rev Immunol. 2009;27:621–668.
- Verity DH, Marr JE, Ohno S, et al. Behçet’s disease, the Silk Road and HLA-B51: Historical and geographical perspectives. Tissue Antigens. 1999 Sep;54(3):213–220.


