And he was right. Once word got out, interest in ECHO HCV by rural providers was immediate, the results were excellent, and wider recognition soon followed. In August 2007, Project ECHO was one of three winners chosen (out of 300 entrants) to receive the Disruptive Innovation in Healthcare Award, sponsored by the Robert Wood Johnson Foundation. The award, citing the ingenuity of this “one-to-many” knowledge network, included a $5-million grant for the continued operation and expansion of the ECHO program.
ECHO Rheumatology
Entering its fifth year in operation, and under the guidance of Arthur Bankhurst, MD, professor of medicine and chief of rheumatology at UNMHSC, the ECHO rheumatology section has made significant inroads down many an unpaved lane. “Long ago I recognized the limitation of the rheumatology subspecialty practice throughout the state,” Dr. Bankhurst says. Reasons for this vary, although many are financial. Regardless, the average age for rheumatologists here and nationwide is 55 to 60, he notes. “For the next generation, there is going to be an increasing lack of the rheumatology subspecialty most anywhere you go.” Compounding this dearth in New Mexico is distance. It is not unusual for Dr. Bankhurst to see patients who are driving 600 miles round-trip for the privilege, and this after a months-long wait just to get in. “When I spoke to Dr. Arora about these issues, he very graciously invited me into the ECHO network,” Dr. Bankhurst says.
As with HCV, training in rheumatology would be based on the rudiments of standards of care. “My goal was to see to it that the most common rheumatologic patient problems (uncomplicated cases) could be treated at a distance just as well as they could be in my clinic,” Dr. Bankhurst says. A majority of these connective tissue–disease problems, he estimated, could be handled at a distance by prescribing medications that ordinarily a general practitioner, NP, or PA would be reluctant to use. The ECHO experience would overcome that barrier.
So what is being taught through ECHO? “Early rheumatoid arthritis [RA] can be a subtle diagnosis, so my first emphasis is instructing on how to be able to recognize signs,” Dr. Bankhurst explains. This includes a review not only of radiographic evidence but of the increasingly available but sometimes difficult to interpret molecular diagnostics associated with rheumatologic disease. Following this, the participant’s general medical knowledge is inculcated with rheumatology protocols. “We instruct on the usual paradigms for treatment,” Dr. Bankhurst says. “If it’s RA, we’re using hydroxychloroquine or methotrexate, as well as the combination of biologic agents.” Once ECHO trained, a provider’s reluctance to treat is supplanted by a familiarity with dosing levels and adverse events. “They can handle it, particularly in RA,” Dr. Bankhurst comments. “If you ever listened in on one of my sessions, you would be surprised at the [specialist] level of sophistication that is quickly developed at these remote sites.” He points out that these sites are now as close as the nearest modem. “Wherever the Internet goes, we can potentially go,” he says.
Getting Started
To initiate any type of ECHO, you have to first speak up. “Dr. Bankhurst and I did a lot of educational outreach,” says Jeanne Boyle, RN, BSN, and executive nurse manager of ECHO at UNMHSC. “To gauge interest in the program, we did presentations all over the state in places like, say, the Bayard Community Health Clinic, where you might be talking to just two people.” Boyle also contacted CEOs of hospitals and sponsors of small clinics, among others. “I even called nurses that I knew—any means available to bring the case for [expanding rheumatology services] to the whole state,” she says.
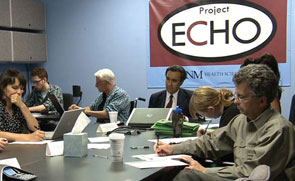
Critical to this effort was attitude, Boyle stresses. “In building grassroots interest, you have to let those folks know that it’s not the academic health science center that’s telling them what they need to do, it’s you asking, ‘How we can serve you?’ ” That’s the core of ECHO.



