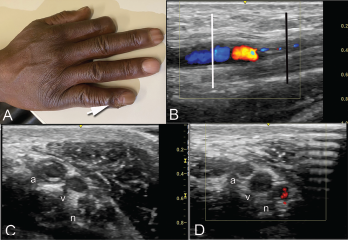
Clockwise from top: Image A shows the periungual ulceration (arrow) of the fifth digit, as well as the prior amputation of the second digit. Image B shows a longitudinal ultrasound of the palmar aspect of the ulnar right wrist. In the center of the image, the ulnar artery is in view and color Doppler flow is visualized within the vessel until there is a reversal of flow demonstrated by color change, followed by severe attenuation of flow distally. Distal to the cessation of flow, the vessel appears hypoechoic due to proliferation of the intima to the point of occluding the lumen. Image C shows a transverse view at the level of white line in Image B, with endothelial proliferation seen around a central lumen of the artery (a), next to the vein (v) and ulnar nerve (n). Image D, shows a transverse view at the level of the black line in Image B, where the arterial lumen (a) is occluded.
A 51-year-old man with a history of limited systemic sclerosis with Raynaud’s phenomenon and pulmonary hypertension being treated with tadalafil and macitentan presented to a clinic with ulceration of his right pinkie. The patient had injured the finger two months earlier. He reported poor healing and the presence of a persistent ulcer since the injury.
The patient had a history of a prior ulceration of the right index finger, which led to an amputation in 2011. He had no history of lower extremity vascular disease, diabetes mellitus or hypertension, but had smoked one pack of cigarettes per day for 20 years, quitting 10 years before.
On exam, a small ulcer was seen at the distal cuticle of the right pinkie, without weeping or expressible material (see Figure 1A). An ultrasound performed on the right upper extremity to evaluate the vasculature of the right hand showed intimal proliferation and vascular occlusion at the level of the pisiform (see Figures 1B, C and D).
The patient received an ulnar nerve block to relieve the pain and help improve perfusion. A surgical referral was placed for a sympathectomy and ulnar artery revascularization.
This patient had macrovascular involvement of the ulnar artery as a manifestation of his systemic sclerosis, which was evidenced by bedside ultrasound showing concentric arterial thickening with decreased blood flow.
Discussion
A hallmark of systemic sclerosis is widespread vascular dysfunction and progressive fibrosis of the skin and internal organs.1 The main vascular complications of systemic sclerosis include Raynaud’s phenomenon with ischemic digital ulcers, pulmonary arterial hypertension and scleroderma renal crisis. These complications occur due to endothelial injury, intimal thickening with narrowing and obliteration of microvasculature.1,2 Although microvascular involvement is a well-known component of the disease, large vessel involvement has also been described, particularly in the ulnar artery.3–6
Using arterial Doppler studies, Stafford et al. showed an increased prevalence of ulnar artery stenosis in more than half of the patients with systemic sclerosis compared with matched controls, with no significant differences between the two groups in other large arteries.3
Ulnar artery narrowing, stenosis and occlusion can reduce perfusion to the digits, leading to ulcers or poor wound healing in scleroderma patients.4 Ulnar artery narrowing can result in infections, surgeries or amputations of the digits, as well as other complications.7
The predictive value of ulnar artery occlusion on ultrasound has been studied by Frerix et al. They found ulnar artery occlusion in 22% of patients with systemic sclerosis.5 Patients with ulnar artery occlusion during follow-up were more likely to develop new or recurrent digital ulcers than patients without ulnar artery occlusion.5
In studies by Lescoat et al., ulnar artery occlusion was found in 37% of patients with systemic sclerosis and was significantly associated with disease duration, history of digital ulcers, worsening diffusing capacity of carbon monoxide (DLCO), higher modified Rodnan skin scores and anti-centromere antibodies.6
The association of ulnar artery occlusions with lower DLCO values, but not with interstitial lung disease, strengthens the relevance of ulnar artery occlusion as a severity marker of vasculopathy in systemic sclerosis, because the decreased DLCO values are more likely secondary to pulmonary artery hypertension.6
Additionally, ulnar artery occlusion is associated with microvascular disease, as assessed by nailfold capillaroscopy, and has a stronger association with digital ulcerations (odds ratio: 10.7) than capillaroscopic abnormalities.8
Ulnar artery revascularization was reported to produce dramatic improvement in the healing of digital ulcers in eight patients with severe scleroderma-related vasculopathy.4 Because ulnar artery occlusion can predict development of digital ulcers in patients with systemic sclerosis, ultrasound may be useful for patient selection into trials for the treatment of vasculopathy.
In Sum
This case highlights the value of hand ultrasound for rheumatologists treating patients with systemic sclerosis.
Devin Marie Driscoll, MD, PGY2, is an internal medicine resident, Boston Medical Center.
Andreea M. Bujor, MD, PhD, is an assistant professor, Arthritis and Autoimmune Diseases Research Center, Boston University School of Medicine.
Eugene Kissin, MD, RhMSUS, is a clinical professor of medicine, Boston University School of Medicine.
References
- Fleischmajer R, Perlish JS, Shaw KV, et al. Skin capillary changes in early systemic scleroderma. Electron microscopy and in vitro autoradiography with tritiated thymidine. Arch Dermatol. 1976 Nov;112(11):1553–1557.
- Grassi W, Core P, Carlino G, et al. Labial capillary microscopy in systemic sclerosis. Ann Rheum Dis. 1993 Aug;52(8):564–569.
- Stafford L, Englert H, Gover J, et al. Distribution of macrovascular disease in scleroderma. Ann Rheum Dis. 1998 Aug;57(8):476–479.
- Taylor MH, McFadden JA, Bolster MB, et al. Ulnar artery involvement in systemic sclerosis (scleroderma). J Rheumatol. 2002 Jan;29(1):102–106.
- Frerix M, Stegbauer J, Dragun D, et al. Ulnar artery occlusion is predictive of digital ulcers in SSc: A duplex sonography study. Rheumatology (Oxford). 2012 Apr;51(4):735–742.
- Lescoat A, Yelnik CM, Coiffier G, et al. Ulnar artery occlusion and severity markers of vasculopathy in systemic sclerosis: A multi-center cross-sectional study. Arthritis Rheumatol. 2019 Jun;71(6):983–990.
- Sunderkotter C, Herrgott I, Bruckner C, et al. Comparison of patients with and without digital ulcers in systemic sclerosis: detection of possible risk factors. Br J Dermatol. 2009 Apr;160(4):835–843.
- Lescoat A, Coiffier G, de Carlan M, et al. Combination of capillaroscopic and ultrasonographic evaluations in systemic sclerosis: Results of a cross-sectional study. Arthritis Care Res (Hoboken). 2018 Jun;70(6):938–943.


