Other Meet the Professor sessions at the 2019 Annual Meeting will include:
- Musculoskeletal Radiology: Pearls for the Rheumatologist—speaker John A. Carrino, MD, MPH, vice chair of radiology at the Hospital for Special Surgery, will discuss a wide array of imaging options for diagnosis of arthropathies, including uncommon or rare diseases, and how to interpret findings that may overlap with multiple diagnoses, as well as how rheumatologists may work with radiologists to manage these cases;
- CNS Vasculitis and Its Impostors—speaker Rula Hajj-Ali, MD, staff physician at Cleveland Clinic’s Center for Vasculitis Care and Research, will conduct a case-based, interactive discussion about the diagnosis and optimal management of primary and secondary central nervous system vasculitis and address how to distinguish it from mimics; and
- Management of Rheumatic Disease Patients Undergoing Arthroplasty—speaker Susan M. Goodman, MD, a rheumatologist at the Hospital for Special Surgery, will discuss evidence on perioperative complications, including venous thromboembolism, infections and periprosthetic fracture, for patients with various rheumatic diseases who have total hip or knee replacement. The talk will clarify the rationale behind management options and make it easier to discuss treatment choices with patients.
Workshops: Refine Skills
One of the new Workshops this year is Hands-On Approach to Perform Salivary Gland (Lip) Biopsy, with instructors Robert W. Ike, MD, associate professor of medicine at the University of Michigan, Ann Arbor, and Sara S. McCoy, MD, assistant professor of medicine, University of Wisconsin School of Medicine and Public Health, Madison. They will review the indications, risks and histopathologic interpretation of minor salivary glands, then devote most of the session to practicing biopsy techniques.
Rheumatologists may not be comfortable with small procedures, such as mucosal incisions and simple sutures, says Dr. McCoy.
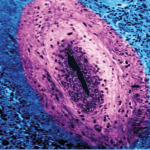
“We will recreate an environment in which rheumatologists can practice their technique on animal-model simulations. The end goal of this workshop is to make rheumatologists comfortable with the utilization of the minor salivary gland biopsy in their practice,” she says. “The minor salivary gland biopsy is a major part of diagnostic criteria for Sjögren’s syndrome and can serve clinically to differentiate seronegative Sjögren’s syndrome patients from patients with xerostomia and no systemic autoimmune disease.”
Minor salivary gland biopsy may be used to evaluate patients for Sjögren’s mimics, such as sarcoidosis and lymphoma, and for prognostication regarding risk of lymphoma in Sjögren’s syndrome. “Despite the clinical relevance of the minor salivary gland biopsy, the process of referring patients outside of rheumatology for biopsy is time-intensive and costly to patients,” says Dr. McCoy. “By providing the biopsy as part of standard rheumatology office practice, we can improve the cost and convenience of this procedure for our patients.”