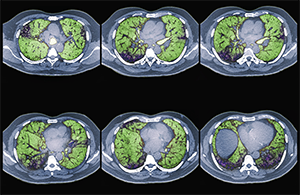
Colored CT scans of axial sections through the chest of a 68-year-old patient with ILD.
Zephyr/ScienceSource.com
SAN FRANCISCO—Interstitial lung disease (ILD) represents a heterogeneous group of disorders characterized by inflammation or fibrosis of the lungs. The disorders are also associated with a spectrum of connective tissue diseases (CTDs).
ILD is a common manifestation of CTDs, such as scleroderma, poly-/dermatomyositis and rheumatoid arthritis—and is a leading cause of morbidity and mortality in these conditions, said Aryeh Fischer, MD, associate professor of medicine in the Divisions of Rheumatology and Pulmonary Sciences at the University of Colorado, during a full-day conference devoted to ILD sponsored by the University of California-San Francisco on Nov. 5, 2016.
“It is important to consider the intersection of CTD and ILD as a spectrum of diseases. Inherently, we believe these conditions each likely behave differently and may respond to treatment differently,” said Dr. Fischer.
Aryeh Fischer, MD
The recognition that an ILD is associated with CTD affects prognostication and management, and provides a clinical context for understanding extrathoracic manifestations of disease. A diagnosis of a CTD can also address some of the frustrations ILD patients feel about being labeled “idiopathic.” Roughly 30% of patients presenting to an ILD center presumed to have an idiopathic ILD will have an underlying CTD as the cause of their ILD, Dr. Fischer noted.
Many patients with ILD have subtle features suggestive of an autoimmune etiology, but current strategies and even terminology for identifying and classifying these patients can be controversial and inadequate, he said. What about ILD patients who present without any extra-thoracic symptoms? According to traditional classifications, they are not considered to be “rheumatologic” patients, but Dr. Fischer led a joint European Respiratory Society and American Thoracic Society task force that recently proposed a new classification category, “interstitial pneumonia with autoimmune features” (IPAF).1
The multidisciplinary approach is the gold standard for diagnosing and treating these conditions, speakers noted, and the conference illustrated that approach with a panel discussion comprising a pulmonologist, radiologist, pathologist and rheumatologist. Dr. Fischer, the rheumatologist, said he became professionally intrigued by the intersection between the two disease categories. “I have been fortunate to find a home at a respiratory center at the University of Colorado as part of a multidisciplinary ILD program.”
To Biopsy or Not
How do you diagnose these conditions? Be a really good clinician, speakers noted. But expect it to be a challenge. “Before we conclude that an ILD is CTD related, we need to consider alternate etiologies. Does the ILD pattern fit? What else could have caused the lung disorder?” Dr. Fischer posed.
Often, a thorough medical history and physical examination combined with a high-resolution CT scan can answer the diagnostic question, said Brett Elicker, MD, associate professor of radiology at UCSF. The high-resolution CT scan remains the modality of choice for detecting ILD in CTD and guiding future workups.
Speakers at the conference also presented a range of viewpoints on the risks and benefits of performing diagnostic lung biopsies in patients with CTD-ILD. “In the current era, we often do not perform a lung biopsy unless it’s going to impact treatment,” Dr. Fischer said. “Where I do recommend them is for idiopathic patients where you’re not clear on the etiology or in CTD patients with compelling concerns for an alternative cause, such as hypersensitivity pneumonitis.”

Harold Collard, MD
“I view surgical lung biopsy as a low-risk intervention—but not no risk,” added Harold Collard, MD, director of the ILD program at UCSF. He also highlighted alternate approaches to traditional video-assisted thoracoscopic surgery, including transbronchial cryobiopsy, which allows harvesting of up to 1 cm samples of tissue endoscopically.2
There are few research-supported treatments for many of the conditions under the CTD-ILD umbrella, Dr. Fischer said. Rheumatologists may look to scleroderma with lung involvement as a model for the treatment of other CTDs, because more is known about it. “I’m a rheumatologist—we often treat our patients with corticosteroids. But these are not good for the long term. So we look for steroid-sparing agents, as with any other rheumatologic condition.”
Rheumatologists also recommend immunosuppressive treatments for CTD-ILD conditions. One of those is cyclophosphamide, Dr. Fischer said. “If I use it, I use it short term and intravenously.” Other common treatments include azathioprine and mycophenolate mofetil, which has gained popularity as a potential glucocorticoid-sparing agent for the treatment of patients with a diverse spectrum of CTD-ILD.
Two drugs approved in recent years for the treatment of idiopathic pulmonary fibrosis, nintedanib, a tyrosine kinase inhibitor, and pirfenidone, an anti-fibrotic agent, are in various stages of clinical trial investigation for potential treatment of fibrotic ILD in CTD patients.
Non-Pharmaceutical Approaches
Jeffrey Golden, MD
For lung conditions that often cannot be cured—only managed or stabilized—non-pharmacologic treatments are an important component of comprehensive ILD care, Dr. Collard said. “The suffering of these patients cannot be overestimated. But non-pharmacologic interventions can positively impact how they feel.”
Pulmonary rehabilitation is a comprehensive intervention, based on a thorough patient assessment, that incorporates exercise and conditioning, education and behavioral change. Support groups are valued by ILD patients because they feel they are not so alone, with support from others who understand what they are going through.
“A diagnosis of ILD is a real blow to patients and families. What they want and need is information about the disease, its treatment and expected course,” Dr. Collard said. “Once they are past the shock of the initial diagnosis, they want information about how to live with the disease.”
A palliative care approach can be helpful from the point of diagnosis, with an evaluation for hospice eligibility when the disease becomes less manageable. Palliative care offers a range of support with symptoms, fears, financial burdens and spiritual or existential distress.
Lung transplant is the ultimate treatment for severe incurable lung disease, said Jeffrey Golden, MD, associate medical director of the Lung Transplantation Program at UCSF. The number of lung transplants performed annually worldwide is now up to 4,000, and more than half of them have been for CTD-ILD patients, he said. “You want people on the lung allocation list who have the best chance to get a transplant, but who aren’t so sick that it’s futile. If you have somebody with a diagnosis of ILD who could be a candidate, they should contact a transplant program for an informational evaluation session.”
Larry Beresford is a freelance medical journalist in Oakland, Calif.
References
- Fischer A, Antoniou KM, Brown KK, et al. for the ERS/ATS Task Force on Undifferentiated Forms of CTD-ILD. An official European Respiratory Society/American Thoracic Society research statement: Interstitial pneumonia with autoimmune features. Eur Respir J. 2015 Oct;46(4):976–987.
- Hagmeyer L, Theegarten D, Wohlschläger J, et al. The role of transbronchial cryobiopsy and surgical lung biopsy in the diagnostic algorithm of interstitial lung disease. C Clin Respir J. 2016 Sep;10(5):589–595.


