ACR CONVERGENCE 2020—Part of a scientific session on Monday, Nov. 9, focused on the use of various rheumatology therapies as repurposed treatments for the atypical cytokine storm syndrome that occurs in some people with COVID-19. Roberto Caricchio, MD, chief of the Division of Rheumatology at Lewis Katz School of Medicine, Temple University, Philadelphia, spoke to ACR colleagues about the characteristics of this syndrome, the rationale behind therapeutic use of these treatments and what has been learned.
Of the numerous clinical trials now taking place for COVID-19, a significant subset are for therapies sometimes used in rheumatology: small-molecule, disease-modifying anti-rheumatic drugs, such as baricitinib; and biologics, such as those blocking interleukin 1 (IL-1) and IL-6. For the most part, these therapies have been selected not for antiviral properties, but for their potential capacity to calm cytokine storm syndrome secondary to COVID-19. Dr. Caricchio explained, “The rationale for using [them] is solid because of the demonstrations we have seen many times over the past several months of an overly exuberant immune response.”
Dr. Caricchio is the principal investigator for several clinical trials related to COVID-19, including one sponsored by Eli Lilly for the JAK1/JAK2 inhibitor baricitinib and a trial with Swedish Orphan Biovitrum studying the anti-interferon gamma antibody emapalumab and the IL-1 antagonist anakinra. He and other colleagues with expertise in cytokine storm published a paper in early April regarding its immunopathology in the context of COVID-19.1 “We thought that—given the data from Europe and from China—there was certainly a hyperinflammatory response ongoing,” he related.
Cytokine Storm Differences
Cytokine storm represents a family of related syndromes with some overlapping pathophysiological signals and some important differences. It can occur due to infectious diseases, such as COVID-19 or influenza; malignancy; chimeric antigen receptor T cell therapy (CAR-T therapy), or from such genetic syndromes as hemophagocytic lymphohistiocytosis (HLH). It can also occur from macrophage activation syndrome (MAS), as a sequela of systemic juvenile idiopathic arthritis or other autoimmune disease. In all cases, uncontrolled immune activation leads to excessive release of multiple cytokines, leading to hyperinflammation and severe multi-organ disease.1
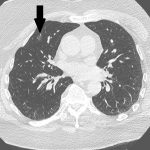
Because of differences in the somewhat atypical cytokine storm seen in COVID-19, Dr. Caricchio et al. proposed a new set of predictive criteria for cytokine storm somewhat distinctive from the criteria that have been used in HLH and MAS.2 Unlike in some other forms, cytokine storm secondary to COVID-19 usually manifests with lymphopenia only—and not with two or more cytopenias. Unlike these other forms, organomegaly is uncommon, and in fact the syndrome can cause shrunken lymph nodes and spleen.
Also, even though multiple inflammatory cytokines are dramatically increased in COVID-19 cytokine storm, the increase is often much less than the even higher levels found in cytokine storm from other causes. This may have implications for the potential effectiveness of agents currently undergoing clinical testing for cytokine storm related to COVID-19, some of which have previously been used to treat cytokine storm from MAS, HLH and other causes.1
A possible exception to this pattern is IL-33, which tends to be elevated in COVID-19 to a greater degree than it is in other causes of cytokine storm. Some have suggested that it might prove to be a key driver of the disease’s progression, even before the onset of cytokine storm itself.3 Dr. Caricchio shared that an IL-33 monoclonal antibody is about to enter clinical trials for COVID-19.
Clinical Trial Eligibility
Greater use of specific cytokine storm criteria might also be of benefit in research. Dr. Caricchio noted that many of the therapies in trials for COVID-19-related cytokine storm have lacked stringent stratification in their exclusion and inclusion criteria. He related that patients with viral pneumonia from COVID-19, as well as some form of increased inflammatory measure, such as C-reactive protein or ferritin, were usually found to be eligible, even though these indicators alone might not best capture the class of people these drugs might help.
This could impact overall outcomes of these clinical trials. “There is a subpopulation of individuals who went through these clinical trials who might have benefited, but the majority may have not, because they never fully developed hyperinflammatory syndrome,” said Dr. Caricchio.
Dr. Caricchio said one surprise about the widespread use of these therapies in this application has been their relative safety regarding rates of serious infection, which have been unexpectedly low. “We are very worried about this—we check for a lot of things before starting a monoclonal antibody,” he said, “and here, of course, we just had to give it.” This may be due to the relatively short window of time for which these therapies are used in a COVID-19 trial, in contrast to long-term use for a rheumatologic condition.
Mixed Interim Results
Interim results from several of these trials have been mixed, with some trials suggesting potential reduced time to recovery but others not showing any benefit. Results of many trials are still pending, and some new ones looking at tumor necrosis factor inhibitors and inhibitors of cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) will be underway soon. “The number of biologics being used for COVID-19 is increasing by the day, and so are the reports that we get back from those clinical trials,” said Dr. Caricchio.
But thus far, none of these agents has shown final positive results significant enough to be granted Emergency Use Authorization status by the U.S. Food & Drug Administration. “Despite the demonstrations in vitro and in correlation with the clinical cases, we still need to determine their effectiveness with randomized controlled clinical trials,” added Dr. Caricchio. “I think we should all appreciate the unprecedented spectacular effort from the scientific world, which is still tremendous.”
Ruth Jessen Hickman, MD, is a graduate of the Indiana University School of Medicine. She is a freelance medical and science writer living in Bloomington, Ind.
References
- Henderson LA, Canna SW, Schulert GS, et al. On the alert for cytokine storm: Immunopathology in COVID-19. Arthritis Rheumatol. 2020;72(7):1059–1063.
- Caricchio R, Gallucci M, Dass C, et al. Preliminary predictive criteria for COVID-19 cytokine storm. Ann Rheum Dis. 2020 Sep 25. [Epub ahead of print].
- Zizzo G, Cohen PL. Imperfect storm: Is interleukin-33 the Achilles heel of COVID-19? Lancet Rheumatol. 2020 Oct 9.