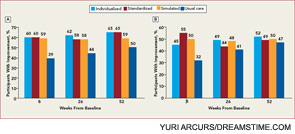
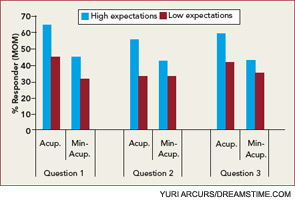
With regard to efficacy, many trials express pain reduction data as means of the experimental groups and do not reveal what proportion of subjects had a positive response and whether the response was clinically meaningful. The data available indicate a positive response rate of 50% or less.4-7,10-12,14 The magnitude of analgesia has varied widely, from large to minimal, and it may be related to some aspects of the experimental protocol, such as whether the subjects were informed that they might receive placebo acupuncture.14 Most adverse events are minor, such as pain and bruising at the site of needle insertion, but the reporting of adverse events has not met the Consolidated Standards of Reporting Trials guidelines.36 Another safety consideration is that acupuncturists trained in traditional Chinese medicine frequently recommend the concomitant use of herbal medicines, which may expose patients to severe adverse events, such as aristolochic acid nephropathy.37-39 A course of acupuncture treatments is usually recommended, and at $50–$100 per treatment, the cost is appreciable.
Recommendation of acupuncture without disclosure that it appears to be a placebo treatment violates ethical guidelines about deception of patients.40-42 Even with altruistic motivation, deception deprives the patient of full autonomy in making informed decisions about healthcare. It may also undermine trust in the physician and jeopardize future consultations and adherence to treatment recommendations.
Despite these ethical concerns, surveys have revealed that 50% or more of physicians in the United States, Denmark, and Israel frequently use placebos in practice.43-46 In one trial, 50% of the physicians were rheumatologists.43 In this context, the designation placebo means a treatment that is not considered to have a specific effect for the medical condition. The placebo treatments included over-the-counter analgesics, sedatives, vitamins, antibiotics for nonbacterial infections, and saline injections or infusions. The reasons for giving the treatment include placating patients and avoiding confrontations. The information given to patients included statements such as, “this is a substance that may help and will not hurt,” or “a medicine not typically used for your condition but might benefit you.” Fewer than 5% of physicians disclosed that the medicine was a placebo, and the use of placebos was considered ethically acceptable by a majority of physicians who used them.
What advice should rheumatologists give to patients with OA of the knee concerning acupuncture treatments? After making sure that the patient understands the chronic nature of the problem, the benefits of conventional measures, especially nonpharmacologic modalities, in reducing pain and maintaining function should be emphasized strongly. Our enhanced knowledge of the power of patient–provider interactions should be used in a nondeceptive manner to convey to the patient our concern, sympathy, and expectations for improvement. In view of the chronic nature of OA, a likelihood of 50% or less that pain will be relieved, the limited duration of the relief, the cost of treatment, and ethical considerations, I would not recommend acupuncture as an adjunctive treatment.

