The role of B cells in autoimmune inflammatory diseases is emerging as one of the most interesting, if not controversial, topics in the development of targeted therapies. This has been highlighted recently by the announcement of a second positive trial of a B cell–targeted treatment in systemic lupus erythematosus (SLE) and by another report of progressive multifocal leukoencephalopathy (PML) in a rheumatoid arthritis (RA) patient treated with rituximab. The diseases considered for B cell–targeted therapy run the spectrum from traditionally viewed B cell–centric diseases such as SLE, to RA, to conventionally viewed T cell–mediated conditions such as multiple sclerosis (MS) (see Table 1). Correspondingly, there are an increasing number of B cell–directed therapies in development for the treatment of autoimmune disease.
B-cell depletion therapy is now routinely used in the treatment of diverse diseases, especially those refractory to conventional immunosuppressive therapy. Moreover, what once was viewed as a one-time therapy often is now used recurrently. It is critical to understand the impact of B-cell depletion on normal immune responses, the reasons B cell–targeted therapies may be efficacious in such a broad range of diseases, potential differences in B cell–directed therapies in efficacy and mechanism of action, and determination as to whether there are subsets of patients who will respond particularly well to B-cell approaches as opposed to other treatment modalities.
The Multi-layered Role of B Cells in Autoimmune Disease
To understand the efficacy of B-cell therapies, as well as treatment response heterogeneity, we need to consider the role of the B cell in autoimmune diseases. As a starting point, to borrow a phrase, autoimmune diseases are not created equal. Certain diseases may be predominantly autoantibody mediated, others may involve B cells via autoantibody-independent mechanisms such as cytokine production or antigen presentation, other disease may be T cell driven, and many undoubtedly represent some combination of these.
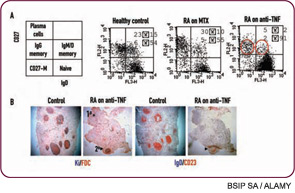
The importance of antibody-independent roles for B cells is often underappreciated, but is highlighted by certain important findings: 1) In mouse lupus, B cells are critical to the development of disease even when they are unable to secrete autoantibodies1; 2) In at least some human autoimmune diseases, the efficacy of B-cell depletion is dissociated from changes in levels of autoantibodies; and 3) The most compelling efficacy data for B-cell depletion occurs in diseases that are traditionally viewed as T-cell driven (e.g., RA and MS), suggesting a role for B cells in regulating other immune cells.
