Rheumatologists and researchers who consider the Health Assessment Questionnaire (HAQ) the gold standard for measurement of self-reported health status may not want to give it up for a new system. However, the person who was instrumental in creating and launching the HAQ in 1980 says that the time is coming when it can be replaced with something much better, thanks to the National Institutes of Health (NIH)–funded Patient Reported Outcomes Measurement Information System (PROMIS) initiative.
James Fries, MD, professor of medicine at Stanford University School of Medicine in Stanford, California, is widely credited with creating the HAQ and is now a principal investigator on PROMIS. Since 2004, the PROMIS research initiative has been working to create a system of highly reliable, precise measures that can be used in clinical studies and in clinical practice to assess patient-reported health and wellbeing across a wide spectrum of chronic diseases and conditions.
PROMIS is in its second phase of funding and includes over 100 researchers at 13 sites. Studies at three of those sites are headed by rheumatologists: Dr. Fries at Stanford; Dinesh Khanna, MD, MS, associate professor of medicine and director of the scleroderma program at the University of Michigan in Ann Arbor; and Esi Morgan DeWitt, MD, MSCE, assistant professor in the division of pediatric rheumatology at Cincinnati Children’s Hospital Medical Center.
“Everyone is used to the HAQ,” Dr. Fries says. “Everyone knows what a patient looks like with a HAQ score of 0.8 and what that means when they read it in an article. The downside of introducing a new [instrument] is that we are saying that this new one is going to be better and will be enough better that you ought to be willing to make the change.”
Because of the years of work and new methodology used by PROMIS researchers, the “infrastructure of clinical science is improving,” representing a “shift in the paradigm about how you measure outcomes in rheumatic diseases. It’s an evolutionary shift, but its time has come,” Dr. Fries says.
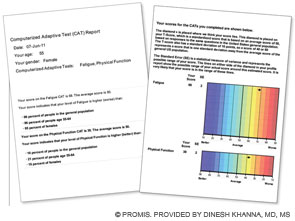
First section (left): Patient’s score for fatigue (where a higher score is worse) and physical function (where a higher score is better); her score is compared with the U.S. general population of women of the same age.
Second section (right): Graphic data showing that the patient’s fatigue is 1.8 standard deviations (SD) below the U.S. general population and that her physical function is 1.2 SD below the U.S. population.
This data can be used by the patient and her physician to establish her baseline self-reported health and in follow-up visits.
New Initiative Versus the Legacies
The HAQ was a “conceptualized” instrument, according to Dr. Fries. “We conceptualized the five D’s: death rates, disability levels, discomfort levels or pain, drug side effects, and the dollar cost. These would encompass all things that would be very important in the treatment of rheumatoid arthritis. … We used common sense to develop it as opposed to any science, and it transformed rheumatology.”