Data from a new study by researchers at the Mayo Clinic in Rochester, Minn., show that patients with rheumatoid arthritis (RA) are more likely to develop reduced kidney function over time compared with people without RA, highlighting the need for rheumatologists to be attentive to the risk of kidney dysfunction in their RA patients.1
“Rheumatologists should monitor kidney function in their patients as appropriate for their age, treatments and comorbidities,” says senior author of the study, Eric L. Matteson, MD, MPH, chair, Division of Rheumatology and professor of medicine, Divisions of Rheumatology and Epidemiology, Mayo Clinic College of Medicine, Rochester, Minn., emphasizing that control of the underlying inflammatory disease is key to reducing the comorbidity of kidney dysfunction related to RA.
Although it is known that various conditions associated with RA, such as hypertension and amyloidosis, and certain drugs affect kidney function, epidemiologic data on the frequency of kidney dysfunction in patients with RA are lacking.
The Study
To fill this gap, Matteson and colleagues retrospectively reviewed data on 813 patients with adult-onset RA and a comparison cohort of 813 without RA in a Minnesota county between 1980 and 2007 to compare the cumulative incidence of reduced kidney function between the two cohorts.
Patient characteristics were largely similar between the two cohorts, with 68% women, a mean age of 56 years, and 9% having reduced kidney function at baseline. The only significant difference was in smoking status, with 45% of RA patients who had never smoked compared with 54% of non-RA patients (P=0.002) who had never smoked. Patients with RA also tended toward a higher mean baseline estimated glomerular filtration rate (eGFR) compared with non-RA patients (86 vs. 83 mL/min/1.73 m2; P=0.008).
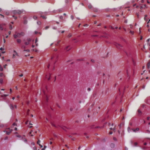
Reduced kidney function was defined using consecutive creatinine measurements at least 90 days apart (e.g., eGFR <60 mL/min/1.73 m2 and eGFR <45 mL/min/1.73 m2 on two consecutive occasions at least 90 days apart). Other outcomes of the study that were assessed included cardiovascular disease (e.g., myocardial infarction, revascularization procedures, angina and heart failure) and death.
The study found a significantly higher 20-year cumulative incidence of reduced kidney function (measured by eGFR <60 mL/min/1.73 m2) in the RA patients compared with non-RA patients (25% vs. 20%, P=0.03). No difference between the two cohorts was found for the development of more advanced kidney disease (measured by eGFR <45 mL/min/1.73 m2) (9% vs. 10%, P=0.8).
Risk Factors
A number of risk factors were found to be significantly related to reduced kidney function, many of which were associated with cardiovascular disease (CVD) and related risk factors (see Table 1). Patients with CVD at baseline had a nearly twofold increased risk of developing reduced kidney function as measured by eGFR <60 mL/min/1.73 m2.
When looking at the risk of developing CVD in patients with reduced kidney function, the study found that RA patients with more advanced kidney disease (eGFR <45 mL/min/1.73 m2) had a significant increased risk of developing CVD (HR, 1.93; 95% CI, 1.04–3.58; P=0.04). No significant association was found between eGFR <60 mL/min/1.73 m2 and the development of CVD in either cohort.
Monitor Patients Closely
Along with close monitoring of kidney function and controlling the underlying inflammatory disease, Dr. Matteson encouraged rheumatologists to help advise patients to use nonsteroidal antiinflammatory drugs (NSAIDs) sparingly.
Mary Beth Nierengarten is a freelance medical journalist based in St. Paul, Minn.