Editor’s note: This article originally appeared in The Rheumatologist in a two-part series in February and April 2009. The topic and this article remain highly relevant, and Dr. Schur has updated it here.
Laboratory testing is an essential element in the diagnosis and management of patients with rheumatic disease. This article focuses on a diverse array of serological markers that can provide unique information on the status of the patient’s immune system that is important in clinical evaluation as well as scientific inquiry. These tests help in the diagnosis of a particular disease, and importantly, they may help monitor disease activity. Indeed, immunological testing represents one of the bedrocks of rheumatology and is a distinguishing feature of our specialty.
Although there are many available tests, the approach to serology follows the traditional approach of any laboratory study. Critical in the interpretation of any serological test is determining its sensitivity (i.e., that proportion of patients with the target disorder who have a positive test), specificity (i.e., that proportion of patients who are free of the target disorder and have negative or normal test results), and positive and negative predictive values, which calculate the likelihood that disease is present or absent based on test results using the test’s sensitivity, specificity and the probability of disease before the test is performed (pretest probability). This review covers data on antinuclear antibodies (ANAs) and tests for rheumatoid arthritis (RA).
Antinuclear Antibodies
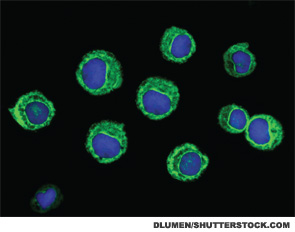
ANAs are the signature autoantibodies of the rheumatic disease and are tested in many clinical scenarios.1-3 These antibodies are usually detected by immunofluorescent (IF) techniques, utilizing Hep-2 cell lines, and specific antinuclear antibodies are detected by solid-phase immunoassays—for example, an ELISA. One hundred and eighty autoantibodies have been described so far in patients with systemic lupus erythematosus (SLE).58 The IF ANA is generally screened at a dilution (i.e., titer) of 1:40, and, if positive, serial dilutions are carried out until a dilution is negative. Most labs titer to 1:1280, but some go higher. It is not clear whether titering higher is clinically useful, because the titer of an ANA usually does not correlate with clinical activity.
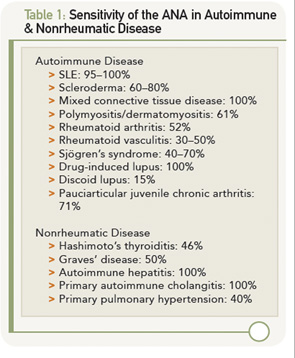
The IF ANA test is especially useful as an initial screen for patients suspected of having systemic lupus erythematosus (SLE). ANA testing is also useful for the evaluation of patients with other suspected rheumatic conditions including Sjögren’s syndrome, mixed connective tissue disease (MCTD), drug-induced lupus erythematosus, dermato-/polymyositis, scleroderma, adult and juvenile arthritis and autoimmune hepatitis. However, the presence of an ANA does not signify the presence of illness, because these antibodies may also be found in otherwise normal individuals. As shown in Table 1 (left), the sensitivity of the ANA for a particular autoimmune disease can vary widely.
Other well-recognized conditions that are occasionally associated with a positive ANA include chronic infectious diseases, such as mononucleosis, subacute bacterial endocarditis and tuberculosis; some lymphoproliferative diseases; and up to 90% of patients taking certain medications, especially procainamide and hydralazine, and those patients with rheumatoid arthritis treated with anti-TNF biologicals. However, most of the patients who take these medications and develop a positive ANA test do not develop clinical drug-induced lupus.
False-positive ANAs (i.e., ANAs in the absence of autoimmune disease or other diseases) are commonly found in normal women, elderly individuals and first-degree relatives of patients with ANA-positive autoimmune diseases (typically in low titer). There are several important points about ANA that should be considered in the clinical setting.
- The presence of high concentrations of antibody (titer >1:160) should make one suspicious that an autoimmune disorder is present. In this scenario, I recommend that sera then be tested for antibodies to double-stranded DNA (dsDNA), Sm, RNP, Ro (SS-A), La (SS-B) and, perhaps, Scl-70. The presence of antibodies to any of these greatly increases the likelihood that the patient has SLE, MCTD, Sjögren’s or scleroderma. Some labs will automatically test for these antibodies whenever the screening ANA is positive. However, the presence of these antibodies is not diagnostic of disease. If no initial diagnosis can be made, it is my practice to watch the patient carefully over time for the development of an ANA-associated disease and see the patient at least twice yearly.

- The combination of low titers of antibody (<1:80) and no or few signs or symptoms of disease portends a much smaller likelihood of an autoimmune disease developing. As a result, these patients with low ANA titers need to be reevaluated less frequently—yearly, unless clinical symptoms evolve to suggest an autoimmune disease.
- A patient with a negative ANA is highly unlikely to have either SLE, MCTD, Sjögren’s or scleroderma. However, if there is still strong clinical evidence of a systemic autoimmune disorder, one may test for the specific antibodies to double-stranded (ds) DNA, Sm, RNP, Ro, La or Scl-70, and if present increases the likelihood that they may have one of these autoimmune disorders. However, in my experience, these tests are typically negative. Nevertheless, it is prudent to see such patients where there is a high clinical index of suspicion, at least yearly—although more frequently if clinically indicated.
- Antinuclear antibodies produce a wide range of staining patterns (homogenous, diffuse, peripheral, rim, speckled, nucleolar, anticentromere, etc.). The nuclear staining pattern has been recognized to have a relatively low sensitivity and specificity for different autoimmune disorders. The presence of antibodies directed at specific nuclear antigens is usually more useful. (These antibodies include the following: dsDNA, Sm, RNP, Ro, La or Scl-70.)
Over the past few years, investigators and biotech firms have been developing solid-phase immunoassays to replace the IF ANA test.4-23 The rationale behind this attempt relates to performance characteristics of the IF technique. This test is very labor intensive and is subject to variation due to different interpretations by technicians. Also complicating testing is the fading of the image as it is examined in a fluorescent microscope. Furthermore, the IF technique uses serial dilutions of patient sera, which will give results that may not be linear. Variations in titer by twofold are common in day-to-day testing on the same sample; fourfold differences are said to be “significant.” By contrast, solid-phase immunoassays are automated and highly reproducible. The results are linear, and the technique is less labor intensive and, thus, cheaper to perform.
Because of these considerations, there should be economic savings in employing a solid-phase immunoassay for quantitating an ANA. Thus, in an attempt to develop solid-phase ANA immunoassays, a number of groups have put onto the solid phase whatever antigens are typically assayed in the more specific ANA immunoassays (e.g., DNA, Sm, RNP, Ro/SSA, La/SSB, nucleoprotein, cell extracts, etc.). In published reports, the correlation coefficient between ANA titers and these solid-phase assays is quite good. Thus, many commercial firms have switched their ANAs to these solid-phase immunoassays.4-23 Of concern, however, is the high frequency/percentage of false-negative results in patients with known SLE and related diseases, as well as the continued high frequency of “false positives” (e.g., a positive ANA in someone without SLE) in these studies.15-21 Further work is needed to improve the sensitivity and especially the specificity of these solid-phase immunoassays to ensure that patients with SLE and related diseases are not missed by these solid-phase immunoassays.
Antibodies to DNA
Antibodies to DNA can be primarily divided into those that react with single-stranded (ss) DNA and those recognizing dsDNA.24-26
Anti-ssDNA antibodies have been reported in SLE, rheumatoid arthritis, drug-related lupus, healthy relatives of patients with SLE and, less commonly, in other rheumatic diseases (see Table 2). Thus, anti-ssDNA has limited usefulness for the diagnosis of SLE or other rheumatic diseases. Anti-ssDNA do not correlate well with disease activity and are, therefore, not useful for disease management.
Antibodies to dsDNA are most frequently detected by solid-phase immunoassays, but also in some labs by the crithidia IF assay or occasionally the Farr radioimmunoassay. Most hospital and commercial labs do only one assay. The Farr assay probably has the highest specificity and lowest sensitivity of the three assays for the diagnosis of SLE, and solid-phase assays have the highest sensitivity and lowest specificity; the crithidia assay falls in between. The Farr assay also has the disadvantage of using radioactive material, which most labs shun, and the crithidia test is very labor intensive. I prefer the ELISA assay for everyday use.
Anti-dsDNA are specific (95%) though not highly sensitive (70%) for SLE, making them very useful for diagnosis when positive26 (see Table 2). They are occasionally found in other conditions, including rheumatoid arthritis, juvenile arthritis, drug-induced lupus, autoimmune hepatitis and even in normal persons.
Titers of anti-dsDNA antibodies often fluctuate with disease activity, especially lupus nephritis and are therefore useful in many patients for following the course of SLE. If a patient has a rising titer or very high titer, but clinically is quiescent, I do not treat the serological abnormality, but consider it a warning sign that the patient needs to be followed more closely and treated when something happens clinically to warrant a change in therapy.59 However, some investigators have treated these serological abnormalities (especially when associated with low complement levels) and have reported improved clinical outcomes. Conversely, I use a falling titer in someone who is getting better after a flare on treatment as a guide in reducing treatment (e.g., corticosteroids and/or immunosuppressives).
The association between anti-dsDNA antibodies and other disease manifestations of SLE is far less clear. For example, there is no relationship between anti-dsDNA titer and disease activity of neuropsychiatric SLE.
Distinguishing active lupus manifestations from infectious complications or toxic effects of drugs—and from unrelated disease—is always a challenge. The presence of anti-dsDNA antibodies may be helpful in some patients in making this distinction.
Anti-Smith & Antiribonucleoprotein Antibodies
Antibodies to Smith (Sm) and antiribonucleoprotein (anti-RNP) are most frequently detected by solid-phase immunoassays.24,27
Anti-Sm antibodies are found in only 10% to 40% of patients with SLE, but are very infrequent in patients with other conditions (i.e., they are not sensitive but are highly specific [see Table 2]). Measurement of anti-Sm titers may be useful diagnostically, particularly at a time when anti-DNA antibodies are undetectable. Given the relatively low sensitivity of anti-Sm, however, a negative value in no way excludes the diagnosis of SLE.
Anti-RNP antibodies are found in about 40% to 60% of patients with SLE, but are not specific for SLE, being a defining feature of MCTD. These antibodies can also occur in low titers and low frequencies in other rheumatic diseases, including RA and scleroderma (see Table 2).
Neither the titer (levels) of anti-Sm nor anti-RNP antibodies correlates significantly with any clinical activity.27
Anti-Ro/SSA & Anti-La/SSB Antibodies
Readers may wonder why most authors use the nomenclature Ro/SSA and La/SSB. Antibodies to Ro and La were first described in patients with SLE, and antibodies to SSA and SSB were first described in patients with Sjögren’s syndrome.60,61 Only many years later when these groups collaborated was it recognized that Ro=SSA and La=SSB. Antibodies to Ro/SSA and La/SSB are most frequently detected by solid-phase immunoassays.28,29 Anti-Ro/SSA and anti-La/SSB have been detected in high frequency in patients with Sjögren’s syndrome and in SLE, but also in patients with photosensitive dermatitis and in 0.1% to 0.5% of healthy adults.
Anti-Ro/SSA antibodies are found in approximately 50% of patients with SLE (see Table 2). They have been associated with photosensitivity, subacute cutaneous lupus, cutaneous vasculitis (palpable purpura), interstitial lung disease, neonatal lupus and congenital heart block. Anti-Ro/SSA antibodies are found in approximately 75% of patients with primary Sjögren’s syndrome (see Table 2), and high titers of these antibodies are associated with a greater incidence of extra glandular features, especially purpura and vasculitis. By contrast, Ro/SSA antibodies are present in only 10% to 15% of patients with secondary Sjögren’s syndrome associated with rheumatoid arthritis. Therefore, the presence of Ro/SSA or anti-La/SSB antibodies in patients with suspected primary Sjögren’s syndrome strongly supports the diagnosis.
Approximately 50% of patients with SLE who have anti-Ro antibody also have anti-La antibody, a closely related RNA-protein antigen. Similarly, most patients with Sjögren’s syndrome also have anti-La (SSB) antibodies. It is exceedingly rare to find patients with anti-La antibodies without anti-Ro antibodies.
In my opinion, the indications for ordering an anti-Ro/SSA and anti-La/SSB antibody tests are as follows:
- Women with SLE who are pregnant or may become pregnant in the future;
- Women who have a history of giving birth to a child with heart block or myocarditis;
- Patients with a history of unexplained photosensitive skin eruptions;
- Patients strongly suspected of having SLE but who have a negative ANA test; or
- Patients with symptoms of xerostomia, keratoconjunctivitis sicca and/or salivary and lacrimal gland enlargement.
Antiribosomal P Protein Antibodies
Antiribosomal P protein antibodies have been detected in 10% to 20% of patients with SLE in the United States and 40% to 50% of Asian patients with SLE, but rarely in other rheumatic diseases.30 Antiribosomal P protein antibodies have been detected in patients with lupus-associated psychosis, although not all studies have confirmed this. Depression and renal and liver involvement in patients with lupus have also been associated with antiribosomal P protein antibodies in some small studies.
Because of the low sensitivity and poor clinical correlation, many investigators—including myself—see little clinical usefulness in this test.
Anticentromere Antibodies
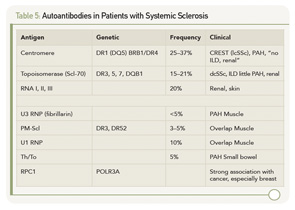
Anticentromere antibodies (ACAs) are found almost exclusively in patients with limited cutaneous systemic sclerosis (lcSSc) especially in those with CREST.31 ACAs have been observed in 57% of patients with CREST but have also been seen in patients with other conditions, including in some patients with Raynaud’s phenomenon alone. ACAs are typically detected by the characteristic IF pattern on Hep-2 cells.
Anti–Scl-70 (topoisomerase-1) Antibodies
Approximately 15% to 20% of patients with scleroderma have antibodies to a 70kd protein (topoisomerase-1), subsequently named Scl-70.31 The usual method for detection is by ELISA. The presence of these antibodies appears to increase the risk for pulmonary fibrosis among patients with scleroderma and is quite specific for the disease.
SLE, Scleroderma & Sjögren’s Syndrome
If one suspects SLE based on the history, physical examination and complete blood count (e.g., leucopenia, thrombocytopenia), request an ANA test. If it is negative, it is highly unlikely that the patient has SLE, and the patient can be reassured. If the titer is <1:160, SLE is unlikely, and the patient can be reassured that SLE is unlikely, but the patient should be followed periodically. A titer of ≥1:160 increases the likelihood of SLE and related disorders. However, it is important to remember that 85% of individuals with a positive ANA do not have SLE. If the ANA is positive, one should also test for antibodies to dsDNA, Sm, RNP, Ro/SSA and La/SSB. The presence of these antibodies greatly increases the likelihood that the patient has SLE and related disorders (see Table 2), and the patient needs to be followed more closely.
The detection of anticentromere and anti–Scl-70 antibodies is very useful for the diagnosis of scleroderma.
The detection of antibodies to Ro/SSA and La/SSB are also useful for the diagnosis of Sjögren’s syndrome.
The only one of these tests that is useful to monitor activity is the anti-dsDNA.
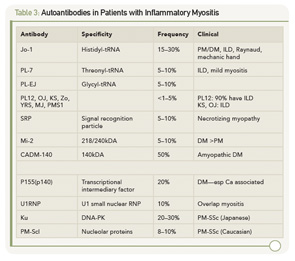
Other antinuclear and related autoantibodies have been described in patients with inflammatory myositis and systemic sclerosis (summarized in Table 3 and Table 4).

Rheumatoid Factors
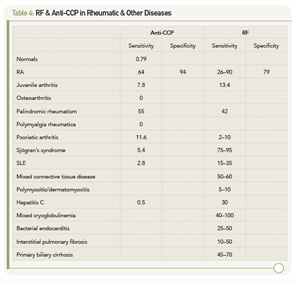
Rheumatoid factors (RFs) are antibodies directed against the Fc portion of immunoglobulin G (IgG). RFs, as currently measured in clinical practice, are usually an IgM RF, although other immunoglobulin types, including IgG and IgA, have been described.32,33 ELISA or nephelometry generally detects the presence of RF; latex agglutination (a test fraught with technical problems) is still sometimes used. Testing for RF is primarily used for the diagnosis of RA; however, RF may also be present in other rheumatic diseases and chronic infections (see Table 5).34
Patients may have detectable serum RF in a variety of rheumatic disorders, many of which share similar features, such as symmetric polyarthritis and constitutional symptoms. These include idiopathic juvenile idiopathic arthritis, palindromic rheumatism and Sjögren’s syndrome (see Table 5).32,33
Nonrheumatic disorders characterized by chronic antigenic stimulation (especially with circulating immune complexes or polyclonal B lymphocyte activation) commonly induce RF production (see Table 5). Included in this group are indolent or chronic infection, as with subacute bacterial endocarditis or hepatitis B or C virus infection, and inflammatory or fibrosing pulmonary disorders, such as sarcoidosis, malignancy and primary biliary cirrhosis. Rheumatoid factors have been found in up to 5% of young, healthy individuals. The reported incidence may be higher in elderly subjects without rheumatic disease, ranging from 3–25%.
The higher the titer, the greater the likelihood that the patient has a rheumatic disease. There are, however, frequent exceptions to this rule, particularly among patients with one of the chronic inflammatory disorders noted above. Further, the use of a higher titer for diagnosis decreases the sensitivity of the test at the same time as it increases the specificity. RF-positive patients with RA may experience more aggressive and erosive joint disease and extra-articular manifestations than those who are RF negative. Similar findings have been observed in juvenile RA. These general observations, however, are of limited utility in an individual patient because of wide interpatient variability. In this setting, accurate prediction of the disease course is not possible from the RF alone. RF titer rarely correlates with the degree of clinical activity.
Antibodies to Citrullinated Proteins
There has been considerable interest in developing a better test for the diagnosis of RA, which has greater sensitivity and specificity than the tests that detect RFs. Within the last decade, as an outgrowth of determining the molecular specificity of antifilaggrin, antikeratin and antiperinuclear antibodies, it was recognized that many patients with RA have antibodies to citrullinated proteins. Proteins that are citrullinated have had an arginine replaced by citrulline, a minor amino acid. This posttranslational modification is mediated by the enzyme peptidyl arginine deiminase 4 (PAD4).
PAD4 is the form of PAD associated with RA. It has been found in bloodstream granulocytes and is localized in the cell nucleus. Its only known activator is a component in cigarette smoke, but its activation is also associated with inflammation. Much more work needs to be done to determine what specifically in RA activates (and downregulates) PAD. Because increased activity of PAD4 has been demonstrated in synovial fluid and synovium of patients with RA and other inflammatory arthritides, but generally not OA, it appears to be associated with inflammation. Citrullination of proteins has also been in noted in multiple sclerosis. The primary physiologic role for PAD enzymes (and the conversion of arginine to citrulline) appears to be related to regulation of nucleosome, that is, histone function. However, the development of antibodies to citrullinated proteins is relatively specific to RA.
To facilitate analysis of antibodies to citrullinated proteins, a number of peptide antigens containing citrulline were created, although these have had a variable degree of sensitivity for recognizing patients with RA. However, a cyclic peptide containing citrulline was found to have a high sensitivity and was subsequently utilized to develop a commercial assay. This test, named anti-CCP (for cyclic-citrullinated peptide) has now been studied extensively, especially in Europe, and it has better sensitivity and specificity for the diagnosis of RA than tests that detect RF; the (positive) predictive value for the diagnosis of RA was 83% for anti-CCP(2), 77% for RF and 83% for the combination of RF and CCP. A number of commercial firms have developed different assays for the detection of these antibodies to CCP, and the assays have been called CCP1, CCP2, CCP3, etc.
There have been numerous claims regarding the superiority of one assay compared with another, and this requires further investigation. In addition, a number of groups have assayed antibodies to other citrullinated proteins—especially fibrinogen and vimentin—and compared these assays to anti-CCP, with variable results. These latter assays are not, at present, commercially available. Most studies to date on examining the frequency, sensitivity, specificity, predictive value of anti-CCP in RA relate to CCP2—which is the assay I employ in my laboratory.
Since the original description of anti-CCP antibodies,35,36 multiple studies have established the clinical utility of measuring these anticitrulline autoantibodies via commercial assays (anti-CCP) as a biomarker in RA.37 In addition to displaying a pooled sensitivity of 67% and specificity of 95% for the diagnosis of RA,38 it is now established that anti-CCP autoreactivity is prognostic for disease severity, radiographic erosions and the early recognition of RA.37,39 Rather than supplanting measurement of RF, the utility of anti-CCP has been demonstrated both by itself and in combination with measurement of serum RF. The consensus that has emerged from these studies is that, although anti-CCP and RF are frequently overlapping in their presence and prognostic significance, they are also independently informative in a significant subset of patients. The differences between subsets of RA patients with distinct autoantibody profiles remains poorly understood.
In addition to performance of these antibodies as a biomarker in the clinical setting, recent evidence suggests a pathogenic association between anticitrulline autoantibodies (measured by the anti-CCP test) and RA.40 Retrospective studies in multiple cohorts have demonstrated that measurable levels of anti-CCP autoantibodies frequently precede development of clinical arthritis with evidence for an increase in frequency and titers proximal to disease onset.41,42 At a population level, recent studies have shown that the presence of anti-CCP correlates with the presence of specific HLA-DR alleles with a particularly strong association with the “shared epitope” genes.43-46 At the level of basic mechanisms, citrullinated peptides from known autoantigens bind more avidly to MHC shared epitope than native peptides and are thereby capable of activating CD4+ T-lymphocytes. This property provides a plausible molecular basis for the genetic association seen in RA patients.47
An additional connection between smoking—a putative environmental trigger for RA—and anticitrulline autoantibodies provides further potential insight into mechanisms of disease evolution. It has long been appreciated that smoking confers an increased risk of RA.48-51 Although this finding has not been replicated in all cohorts, recent studies demonstrate that the increased risk conferred by tobacco exposure is present in the anti-CCP+ subset of subjects,37 and is associated with HLA‑DR alleles.45,46 Further, pulmonary lavage samples from smokers show citrullination of cellular proteins that is not present in nonsmoking subjects, providing a potential source of citrullinated antigens to induce autoantibody production. Moreover, citrulline posttranslational modification of tissue proteins occurs in diseased joints, and joint tissue citrullination levels are markedly elevated in the context of inflammation in both humans and experimental rodents.52-56
Evidence from animal models further supports the potential contribution of anticitrulline antibodies to the pathogenesis of inflammatory arthritis. Recent studies in the collagen-induced arthritis model have demonstrated that anticitrulline autoantibodies are induced by immunization with collagen and that establishing tolerance to citrullinated peptides blocks development of disease.54 Perhaps more compelling evidence for the pathogenic role of these antibodies is the ability to passively transfer anticitrulline antibodies to mice with subclinical arthritis and initiate robust symmetric inflammatory synovitis. Interestingly, passive transfer of anticitrulline antibodies into mice without any inflammatory stimulus does not elicit arthritis, and citrullination of joint tissue proteins is evident in mice with subclinical collagen-induced arthritis (CIA).
Taken together, these observations suggest a new disease model where the combination of anticitrulline antibodies and inflammation-induced citrullination of tissue proteins can conspire to induce an autoimmune inflammatory arthritis.40 The clinical utility of testing for anti-CCP versus RF is summarized in Table 5 (above). The anti-CCP test, although having similar sensitivity for the presence of RA, has much greater specificity. In addition, antibodies to CCP are rarely found in patients with other rheumatic conditions and infectious diseases where RF is more frequently found. Anti-CCP is even found frequently before the diagnosis of RA. These observations suggested that the anti-CCP test was more useful for the diagnosis of RA than are RF tests and was, therefore, incorporated into the new ACR/EULAR Criteria for RA.62
Recently, my colleagues and I have examined a large cohort of patients with early arthritis who were followed for at least six months.57 The substitution of anti-CCP for the ACR classification criteria subcutaneous nodules and erosions improved on the ACR classification criteria for the earlier identification and classification of those patients who eventually developed RA. On the basis of these findings, we recommend that, if one suspects that a patient has RA, one should test for both RF and anti-CCP.
What do we do with these results in our Arthritis Center? We have observed a gradual trend for earlier and more aggressive treatment with disease-modifying antirheumatic drugs (DMARDs) in the patient who presents with a symmetric polyarthritis and sometimes even a monoarthritis, who has a positive anti-CCP test. This approach is in marked contrast with the way the RF test was used, due to the lower specificity of this test in early arthritis in predicting RA. However, we rarely add a biological (e.g., TNF blocker) to the treatment regimen unless the patient has failed two DMARDs, clearly has inflammation and is felt clinically to probably have RA. However, more carefully constructed clinical trials are needed to guide us on when and how to treat the early arthritis patient, because not all of them develop RA.
Summary
What does the future hold? First, in respect to antinuclear antibodies, I predict that testing will become more automated, based on both economic pressures and improvement in solid-phase immunoassays. I suspect this will be coupled with the recognition that systemic lupus erythematosus, scleroderma and Sjögren’s each represent a spectrum of related disorders. I predict that the combination of good clinical description, genetic and epigenetic markers and assays for biomarkers via RNA analysis, proteomics, will better divide up related subsets, resulting in better testing as well as therapy.
With respect to RA, I predict less reliance on the misnamed rheumatoid factor test, better recognition that RA is also probably a spectrum of related diseases (not just seropositive and seronegative RA) and that, likewise, better serological and genetic testing will help define patient subsets. I strongly believe that different subsets of “RA” patients will have antibodies to different citrullinated proteins and that we will end up having a RA-citrullinated panel of tests. Hopefully, this subsetting with coupling of better therapies, probably guided by genomics, will improve treatment.
Progress in rheumatology serology has been slow through the 1940s (RF and LE cell prep), 1950s (ANA and anti-DNA), 1960s (Sm, RNP, Ro, La) and 1990s (CCP). However, the understanding of the genetics of the disorders discussed here—as well as the therapies for them—has been accelerating. Let us hope that the future will bring new and better discoveries.
Peter H. Schur, MD, is professor of medicine at Harvard Medical School and the division of rheumatology, immunology and allergy in the Department of Medicine at Brigham and Women’s Hospital in Boston.
Acknowledgment: I am indebted to the work of many authors of UpToDate in Medicine, whose work provided a useful framework for the development of this paper as well as to Drs. Robert Shmerling, David Lee and Donald Bloch with whom I have written papers/chapters on this same subject.
References
- Bloch D. Measurement and clinical significance of antinuclear antibodies. UpToDate. 2014.
- American College of Rheumatology Ad Hoc Committee on Immunologic Testing Guidelines. Guidelines for immunologic laboratory testing in the rheumatic diseases: An introduction. Arthritis Rheum. 2002;47:429–433.
- Solomon DH, Kavanaugh AJ, Schur PH, et al. Evidence-based guidelines for the use of immunologic tests: Antinuclear Antibody testing. Arthritis Rheum. 2002;47:434–444.
- Sinclair D, Saas M, Williams D, et al. Can an ELISA replace immunofluorescence for the detection of anti-nuclear antibodies?—The routine use of anti-nuclear antibody screening ELISAs. Clin Lab. 2007;53:183–191.
- Avaniss-Aghajani E, Berzon S, Sarkissian A. Clinical value of multiplexed bead-based immunoassays for detection of autoantibodies to nuclear antigens. Clin Vaccine Immunol. 2007;14:505–509.
- Copple SS, Martins TB, Masterson C, et al. Comparison of three multiplex immunoassays for detection of antibodies to extractable nuclear antibodies using clinically defined sera. Ann N Y Acad Sci. 2007;1109:464–472.
- Caramaschi P, Ruzzenente O, Pieropan S, et al. Determination of ANA specificity using multiplexed fluorescent microsphere immunoassay in patients with ANA positivity at high titres after infliximab treatment: Preliminary results. Rheumatol Int. 2007;27:649–654.
- Biagini RE, Parks CG, Smith JP, et al. Analytical performance of the AtheNA MultiLyte ANA II assay in sera from lupus patients with multiple positive ANAs. Anal Bioanal Chem. 2007;388:613–618.
- Gonzalez C, Garcia-Berrocal B, Perez M, et al. Laboratory screening of connective tissue diseases by a new automated ENA screening assay (EliA Symphony) in clinically defined patients. Clin Chim Acta. 2005;359:109–114.
- Eissfeller P, Sticherling M, Scholz D, et al. Comparison of different test systems for simultaneous autoantibody detection in connective tissue diseases. Ann N Y Acad Sci. 2005;1050:327–339.
- Smith J, Onley D, Garey C, et al. Determination of ANA specificity using the UltraPlex platform. Ann N Y Acad Sci. 2005;1050:286–294.
- Martins TB, Burlingame R, von Muhlen CA, et al. Evaluation of multiplexed fluorescent microsphere immunoassay for detection of autoantibodies to nuclear antigens. Clin Diagn Lab Immunol. 2004;11:1054–1059.
- Bernardini S, Infantino M, Bellincampi L, et al. Screening of antinuclear antibodies: Comparison between enzyme immunoassay based on nuclear homogenates, purified or recombinant antigens and immunofluorescence assay. Clin Chem Lab Med. 2004;42:1155–1160.
- Nossent H, Rekvig OP. Antinuclear antibody screening in this new millennium: Farewell to the microscope? Scand J Rheumatol. 2001;30:123–126; discussion 127–128.
- Lopez-Hoyos M, Rodriguez-Valverde V, Martinez-Taboada V. Performance of antinuclear antibody connective tissue disease screen. Ann N Y Acad Sci. 2007;1109:322–329.
- Ghillani P, Rouquette AM, Desgruelles C, et al. Evaluation of the LIAISON ANA screen assay for antinuclear antibody testing in autoimmune diseases. Ann N Y Acad Sci. 2007;1109:407–413.
- Bonilla E, Francis L, Allam F, et al. Immunofluorescence microscopy is superior to fluorescent beads for detection of antinuclear antibody reactivity in systemic lupus erythematosus patients. Clin Immunol. 2007;124:18–21.
- Nifli AP, Notas G, Mamoulaki M, et al. Comparison of a multiplex, bead-based fluorescent assay and immunofluorescence methods for the detection of ANA and ANCA autoantibodies in human serum. J Immunol Methods. 2006;311:189–197.
- Shovman O, Gilburd B, Zandman-Goddard G, et al. Multiplexed AtheNA multi-lyte immunoassay for ANA screening in autoimmune diseases. Autoimmunity. 2005;38:105–109.
- Ulvestad E. Performance characteristics and clinical utility of a hybrid ELISA for detection of ANA. Apmis. 2001;109:217–222.
- Olaussen E, Rekvig OP. Screening tests for antinuclear antibodies (ANA): Selective use of central nuclear antigens as a rational basis for screening by ELISA. J Autoimmun. 1999;13:95–102.
- Homburger HA, Cahen YD, Griffiths J, Jacob GL. Detection of antinuclear antibodies: Comparative evaluation of enzyme immunoassay and indirect immunofluorescence methods. Arch Pathol Lab Med. 1998;122:993–999.
- Gniewek RA, Stites DP, McHugh TM, et al. Comparison of antinuclear antibody testing methods: Immunofluorescence assay versus enzyme immunoassay. Clin Diagn Lab Immunol. 1997;4:185–188.
- Bloch D. Antibodies to DNA, SM, and RNP. UpToDate. 2014.
- Hahn BH. Antibodies to DNA. New Engl J Med. 1998;338:1359.
- Kavanaugh AF, Solomon DH, the American College of Rheumatology Ad Hoc Committee on Immunologic Testing Guidelines. Guidelines for immunologic laboratory testing in the rheumatic diseases: Anti-DNA antibody tests. Arthritis Rheum. 2002; 47:546–555.
- Benito-Garcia E, Schur PH, Lahita R. Guidelines for Immunologic laboratory testing in the rheumatic diseases: Anti-Sm and Anti-RNP antibody tests. Arthritis Rheum. 2004; 51:1030–1044.
- Reichlin M. Clinical significance of anti-Ro/SSA and anti-La/SSB antibodies. UpToDate. October 2008.
- Reveille JD, Sherrer YRS, Solomon DH, et al. Evidenced-based guidelines for the use of immunological laboratory tests: Anti-Ro (SS-A) and La (SS-B): A report from the ACR Ad Hoc Committee on Immunological Testing Guidelines. Submitted for publication.
- Bloch D. Antiribosomal P protein antibodies. UpToDate. 2014.
- Denton CP. Classification of scleroderma. UpToDate. 2014.
- Shmerling RH. Origin and utility of measurement of rheumatoid factors. UpToDate. 2014.
- Shmerling RH, Delbanco TL. The rheumatoid factor: An analysis of clinical utility. Am J Med. 1991;91:528.
- Kavanaugh AF, Solomon DH, the American College of Rheumatology Ad Hoc Committee on Immunologic Testing Guidelines. Guidelines for immunologic laboratory testing in the rheumatic diseases. Anti-DNA antibody tests. Arthritis Rheum. 2002;47:546–555.
- Schellekens GA, de Jong BA, van den Hoogen FH, et al. Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. J Clin Invest. 1998;101:273–281.
- Girbal-Neuhauser E, Durieux JJ, Arnaud M, et al. The epitopes targeted by the rheumatoid arthritis-associated antifilaggrin autoantibodies are posttranslationally generated on various sites of (pro)filaggrin by deimination of arginine residues. J Immunol. 1999;162:585–594.
- Lee DM, Phillips R, Hagan EM, et al. Quantifying anti-cyclic citrullinated peptide titres: Clinical utility and association with tobacco exposure in patients with rheumatoid arthritis. Ann Rheum Dis. 2009;68:201–208.
- Nishimura K, Sugiyama D, Kogata Y, et al. Meta-analysis: Diagnostic accuracy of anti-cyclic citrullinated peptide antibody and rheumatoid factor for rheumatoid arthritis. Ann Intern Med. 2007;146:797–808.
- van der Helm-van Mil AH, Verpoort KN, Breedveld FC, et al. Antibodies to citrullinated proteins and differences in clinical progression of rheumatoid arthritis. Arthritis Res Ther. 2005;7:R949–R958.
- van Gaalen F, Ioan-Facsinay A, Huizinga TW, Toes RE. The devil in the details: The emerging role of anticitrulline autoimmunity in rheumatoid arthritis. J Immunol. 2005;175:5575–5580.
- Rantapaa-Dahlqvist S, de Jong BA, Berglin E, et al. Antibodies against cyclic citrullinated peptide and IgA rheumatoid factor predict the development of rheumatoid arthritis. Arthritis Rheum. 2003;48:2741–2749.
- Nielen MM, van Schaardenburg D, Reesink HW, et al. Specific autoantibodies precede the symptoms of rheumatoid arthritis: a study of serial measurements in blood donors. Arthritis Rheum. 2004;50:380–386.
- van Gaalen FA, van Aken J, Huizinga TW, et al. Association between HLA class II genes and autoantibodies to cyclic citrullinated peptides (CCPs) influences the severity of rheumatoid arthritis. Arthritis Rheum. 2004;50:2113–2121.
- Berglin E, Padyukov L, Sundin U, et al. A combination of autoantibodies to cyclic citrullinated peptide (CCP) and HLA-DRB1 locus antigens is strongly associated with future onset of rheumatoid arthritis. Arthritis Res Ther. 2004;6(4):R303–R308.
- Klareskog L, Stolt P, Lundberg K, et al. A new model for an etiology of rheumatoid arthritis: Smoking may trigger HLA-DR (shared epitope)-restricted immune reactions to autoantigens modified by citrullination. Arthritis Rheum. 2006;54:38–46.
- Lee HS, Irigoyen P, Kern M, et al. Interaction between smoking, the shared epitope, and anti-cyclic citrullinated peptide: A mixed picture in three large North American rheumatoid arthritis cohorts. Arthritis Rheum. 2007;56:1745–1753.
- Hill JA, Southwood S, Sette A, Jevnikar AM, Bell DA, Cairns E. Cutting edge: The conversion of arginine to citrulline allows for a high-affinity peptide interaction with the rheumatoid arthritis-associated HLA-DRB1*0401 MHC class II molecule. J Immunol. 2003;171:538–541.
- Silman AJ, Newman J, MacGregor AJ. Cigarette smoking increases the risk of rheumatoid arthritis. Results from a nationwide study of disease-discordant twins. Arthritis Rheum. 1996;39:732–735.
- Heliovaara M, Aho K, Aromaa A, Knekt P, Reunanen A. Smoking and risk of rheumatoid arthritis. J Rheumatol. 1993;20:1830–1835.
- Uhlig T, Hagen KB, Kvien TK. Current tobacco smoking, formal education, and the risk of rheumatoid arthritis. J Rheumatol. 1999;26:47–54.
- Stolt P, Bengtsson C, Nordmark B, et al. Quantification of the influence of cigarette smoking on rheumatoid arthritis: Results from a population based case-control study, using incident cases. Ann Rheum Dis.;62:835–841.
- Makrygiannakis D, af Klint E, Lundberg IE, et al. Citrullination is an inflammation-dependent process. Ann Rheum Dis. 2006;65:1219–1222.
- Vossenaar ER, Nijenhuis S, Helsen MM, et al. Citrullination of synovial proteins in murine models of rheumatoid arthritis. Arthritis Rheum. 2003;48:2489–2500.
- Kuhn KA, Kulik L, Tomooka B, et al. Antibodies against citrullinated proteins enhance tissue injury in experimental autoimmune arthritis. J Clin Invest. 2006;116:961–973.
- Lundberg K, Nijenhuis S, Vossenaar ER, et al. Citrullinated proteins have increased immunogenicity and arthritogenicity and their presence in arthritic joints correlates with disease severity. Arthritis Res Ther. 2005;7(3):R458–R467.
- Masson-Bessiere C, Sebbag M, Girbal-Neuhauser E, et al. The major synovial targets of the rheumatoid arthritis-specific antifilaggrin autoantibodies are deiminated forms of the alpha- and beta-chains of fibrin. J Immunol. 2001;166:4177–4184.
- Liao KP, Batra KL, Chibnik L, Schur PH, Costenbader KH. Anti-CCP revised criteria for the Classification of Rheumatoid Arthritis. Ann Rheum Dis. 2008;67:1557–1561.
- Yaniv G Twig G, Shor D B-A, et al. A volcanic explosion of autoantibodies in systemic lupus eryhthematosus: A diversity of 180 different antibodies found in SLE patients. Autoimmunity Reviews. 2014; In press.
- Schur PH, Sandson J. Immunologic factors and clinical activity in systemic lupus erythematosus. N Engl J Med. 1968 Mar 7;278(10):533–538.
- Provost TT, Razzaque A, Maddison PJ, Reichlin M. Antibodies to cytoplasmic antigens in lupus erythematosus. Serologic markers for systemic disease. Arthritis Rheum. 1977 Nov-Dec;20(8):1457–1463.
- Alspaugh MA, Tan EM. Antibodies to cellular antigens in Sjögren’s syndrome. J Clin Invest. 1975 May;55(5):1067–1073.
- Aletha D, Neogi T, Silman AJ, et al. 2010 Rheumatoid Arthritis Classification Criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010 Sep;62(9):2569–2581.