Although bronchoalveolar lavage remains a valuable research tool, it may be less useful in the clinic. For technical reasons, the interpretation of bronchoalveolar lavage fluid can be difficult when performed in community-based laboratories. Another disadvantage of this test is the potential for sampling error because generally only one or two sites are lavaged. When performed in a standardized fashion in specialized laboratories, however, it does provide clues to the presence of active ILD.
Lung Biopsy
Open lung biopsy is rarely indicated unless there is clinical concern for other pulmonary conditions that might confound SSc (e.g., bronchiolitis obliterans with organizing pneumonia, sarcoidosis, or aspiration, among others). The predominant histologic pattern of SSc-ILD is a nonspecific interstitial pneumonitis. CT findings in SSc closely resemble those observed in patients with idiopathic nonspecific interstitial pneumonitis.
Echocardiography
Obtain echocardiogram with Doppler at baseline on all newly diagnosed patients, and perform serial studies at intervals, depending upon the patient’s clinical symptoms and the results of their other tests (e.g., DLCO). Echocardiography is an important tool to evaluate the complaint of dyspnea, particularly when PAH is suspected (e.g., in the patient found to have a low DLCO percent predicted with normal or only slightly reduced FVC percent predicted [vide supra]).
In two recent studies conducted in community-based rheumatology practices, the prevalence of PAH as defined by an estimated RV systolic pressure of >40 mm Hg was found to be approximately 25% in SSc and mixed connective tissue disease patients.8,9 Thus, one must have a high index of suspicion for PAH in this patient population.
Echocardiography provides important information about right atrial (RA) and right ventricular (RV) size and function—especially RV systolic pressure. (See Figure 3, page 18.) Congenital heart disease, valvular disease, pericardial effusion, and left-sided heart dysfunction may also be detected.
Right Heart Catheterization
Because the Doppler echocardiogram may overestimate or underestimate RV systolic pressure, right heart catheterization is required whenever PAH is suspected. Right heart catheterization remains the gold standard for accurate diagnosis of PAH and also permits assessment of concomitant left ventricular disease by measuring pulmonary capillary wedge pressure or left ventricular end-diastolic pressure. PAH is defined as a mean pulmonary artery pressure of >25 mm Hg at rest, or >30 mm Hg with exercise, and a normal pulmonary capillary wedge pressure (<15 mm Hg). Diastolic dysfunction is not an uncommon cause for dyspnea in SSc patients. Treatment of diastolic dysfunction differs significantly from that of PAH; therefore, cardiac catheterization is critical for accurate diagnosis and management of the SSc patient with suspected pulmonary vascular disease.
Diagnosis and Management
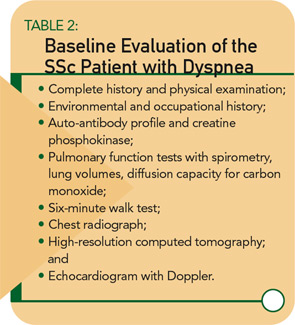
My recommended baseline cardiopulmonary evaluation for a newly diagnosed SSc patient is shown in Table 2. (See above right.) If baseline studies are normal and the patient has no complaints of dyspnea, I recommend annual re-assessment (sooner if the patient develops symptoms). If PFTs are abnormal, further work-up is necessary and should be guided by the particular pattern of PFT abnormalities. For example, a restrictive PFT pattern suggests SSc-ILD, which should be confirmed by CT.