Dr. Piette described pauci-random purpura as fewer than 25 lesions distributed randomly over the body, with occasional clusters on the legs. They are typically formed as a result of ANCA-associated vasculitis or microvascular occlusion, and only rarely are they the result of PLEVA/LyP.
Multi-dependent purpura patterns tend to include more than a 100 purpura. If they are not palpable or partially blanchable, then they are likely caused by platelet-related simple hemorrhage, immune complex vasculitis, or benign hypergammaglobulinemic purpura of Waldenstrom, or are chronic pigmented purpura. If the multi-dependent purpura are palpable or partially blanchable, they probably result from immune complex vasculitis or, more rarely, are chronic pigmented purpura. Purpura that are palpable or partially blanchable may be the result of a disease with secondary hemorrhage.
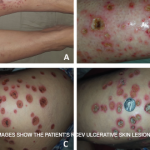
Dr. Piette described the four main purpura patterns—multi-generalized, acral, pauci-random & multi-dependent—& showed examples of each.
Vasculitis Can Mimic Both Simple Hemorrhage & Occlusion
Dr. Piette explained that vasculitis can mimic both simple hemorrhage and occlusion at the clinical and histological level. He then presented slides of purpura and discussed whether the patient had vasculitis, hemorrhage or occlusion. He first presented a patient who had a recurrent crop of lesions that were predominantly macular. Dr. Piette explained that if the purpura burn and occasionally itch, then the patient may have benign hypergammaglobulinemic purpura of Waldenstrom. Such purpura often follow exercise or the ingestion of aspirin or alcohol. They are most common in younger women with no systemic findings.
Urticarial vasculitis also tends to burn more than it itches, and the lesions last longer than 24–48 hours. In this case, the purpura are often minimal and are idiopathic. Urticarial vasculitis may be associated with hepatitis B and hepatitis C infection, as well as systemic lupus erythematosus (SLE). In the case of urticarial vasculitis, history is often more important than biopsy. Consequently, it may be helpful to circle the lesions in order to determine lesional duration. Patients with urticarial vasculitis who have systemic disease or are hypocomplementemic may benefit from a check for C1q antibody.
Conclusion
Dr. Piette explained the initial evaluation of purpura can be done from the doorway. Closer inspection should reveal the morphology of the purpura. The number, distribution and morphology shape the clinical hypothesis. When the data are put together, the physician should be able to propose whether the patient has a simple hemorrhage, inflammatory hemorrhage or occlusion. This clinical hypothesis should then be correlated with additional clinical and laboratory data. He noted, though, that histologic and immune findings can be misleading if the age of the biopsied lesion is not considered in the diagnosis.