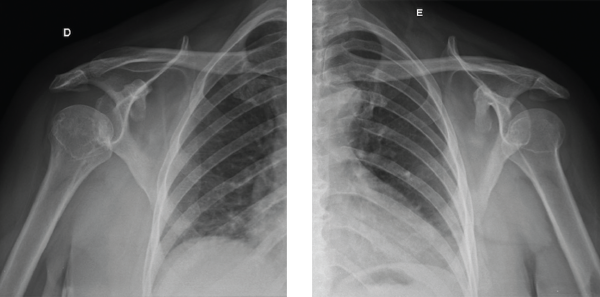
Figure 3: This image shows the patient’s symmetric shoulder dislocations.
degenerative features on both proximal and distal interphalangeal joints (see Figure 6).
All the above features pointed to a neuropathic origin of the patient’s symptoms, suggesting a cervical myelopathy. Magnetic resonance imaging (MRI) of her spine and head were performed, and the MRI confirmed an extensive syringomyelia secondary to Chiari type I malformation (see Figure 7).
What Is NA?
First described in detail by French neurologist Jean Marie Charcot in 1868, the most commonly accepted theory regarding this condition’s development involves the accumulation of minor traumatic events after the

Figure 4: This chest X-ray reveals the dislocation of both humeri.
loss of normal joint sensation. Both sensory (especially those marked by loss of proprioception, thermic and pain sensitivities) and autonomic neuropathy point toward the center of NA’s physiopathology.
Two types of Charcot arthropathy have been described. One is the atrophic form, which is marked by osteopenia, destruction (i.e., the disappearance of bone substance) and dislocation. The other is the hypertrophic variety, which usually presents with upper motor neuron lesions, is less common than the atrophic form and is marked by osteosclerosis and osteophytes, bone fragmentation and absence of osteopenia.
Worldwide, the most common diseases associated with NA include diabetes, syphilis, leprosy and syringomyelia. Depending on the cause, multiple joints may be involved.
In our experience, some Charcot joints suggest a specific etiology for the neuropathy, guiding clinicians to the correct bedside diagnosis. NA involving the shoulders or spine suggests syringomyelia. NA of the feet and ankles suggests diabetes. Charcot arthropathy of the knees points to syphilis. Isolated hand NA suggests leprosy and, to a lesser extent, syringomyelia.
Figures 5A and 5B: These X-rays show incipient reabsorption of the ends of the humeri without the prominence of osteophytes and osteosclerosis.
Although many physicians expect further complementary exams to determine the type of neural injury, we believe a careful history coupled with a physical examination may correctly determine the essential exam physicians must perform, rather than using multiple electroneuromyography and whole-body MRI for the final diagnosis.
Zebras Do Exist!

Figure 6: This X-ray shows degenerative changes on the proximal and distal interphalageal joints and bone reabsortion at the fifth metacarpophalangeal joint of the left hand.
We generally agree with the saying, “When you hear hoofbeats, think horses, not zebras,” but we also teach medical students and fellows to be careful if they are at a safari—in this situation, hoofbeats may really be caused by zebras.