Rheumatoid arthritis (RA) is characterized by polyarthritis, especially involving hands and wrists. Without treatment, RA usually evolves to articular deformities. Unfortunately, although rheumatoid deformities are characteristic, they are not pathognomonic, and we should be aware of possible mimics.1
Neuropathic arthropathy (NA), similar to other diseases, such as hemochromatosis, psoriatic arthritis, calcium pyrophosphate deposition disease, Jaccoud arthropathy, etc., is an example of an RA mimicker.2 This condition, also known as Charcot arthropathy, is marked by progressive joint dislocations and debilitating deformities. Any joint can be involved, depending on the underlying cause of the neuropathy. Although RA may involve the peripheral and central nervous system (mainly via compression, such as carpal tunnel syndrome and cervical myelopathy secondary to atlantoaxial subluxation), the association between RA and NA is so uncommon that every time we come across the possibility of it occurring, we must ask ourselves three questions:3-6
- Is my RA patient experiencing a complication of such a rare situation?
- Is my RA patient experiencing an overlap with another disease that promotes NA?
- Does my patient really have RA?
Case Report

Figures 1 and 2: These images shows the patient’s bilateral ulnar deviation and benediction deformity of the left hand.
Consider the case of a 57-year-old female patient who presented to our rheumatology service to evaluate her for the introduction of biological therapy. She had been diagnosed with RA two years before. Her condition was refractory to methotrexate and leflunomide. Inflammatory markers, including erythrocyte sedimentation rate and C-reactive protein test, were mildly elevated, but she tested negative for rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs). Her complete blood count, electrolytes, urinalysis, renal and hepatic functions, and a viral panel were unremarkable.
The patient referred to mechanical hand pain and multiple unnoticed burn lesions on her upper extremities. Her physical examination was remarkable for benediction hands, ulnar deviation and interosseous muscle atrophy (see Figures 1 and 2), coupled with symmetric shoulder dislocations (see Figure 3, bottom right) and instability.
Her neurologic examination revealed dissociated sensory loss on her hands and arms, as well as limited shoulder abduction secondary to pain. She had already had a chest X-ray to screen for latent tuberculosis during the preparation to use biological therapy, and this radiography was remarkable for dislocation of both humeri (see Figure 4). Shoulder radiography evidenced incipient reabsorption of the ends of the humeri without prominent osteophytes or osteosclerosis characterizing the atrophic form of the Charcot joint (see Figure 5). Hand radiography, in addition to showing the deformities, was remarkable for destructive changes on her right wrist, as well as

Figure 3: This image shows the patient’s symmetric shoulder dislocations.
degenerative features on both proximal and distal interphalangeal joints (see Figure 6).
All the above features pointed to a neuropathic origin of the patient’s symptoms, suggesting a cervical myelopathy. Magnetic resonance imaging (MRI) of her spine and head were performed, and the MRI confirmed an extensive syringomyelia secondary to Chiari type I malformation (see Figure 7).
What Is NA?
First described in detail by French neurologist Jean Marie Charcot in 1868, the most commonly accepted theory regarding this condition’s development involves the accumulation of minor traumatic events after the

Figure 4: This chest X-ray reveals the dislocation of both humeri.
loss of normal joint sensation. Both sensory (especially those marked by loss of proprioception, thermic and pain sensitivities) and autonomic neuropathy point toward the center of NA’s physiopathology.
Two types of Charcot arthropathy have been described. One is the atrophic form, which is marked by osteopenia, destruction (i.e., the disappearance of bone substance) and dislocation. The other is the hypertrophic variety, which usually presents with upper motor neuron lesions, is less common than the atrophic form and is marked by osteosclerosis and osteophytes, bone fragmentation and absence of osteopenia.
Worldwide, the most common diseases associated with NA include diabetes, syphilis, leprosy and syringomyelia. Depending on the cause, multiple joints may be involved.
In our experience, some Charcot joints suggest a specific etiology for the neuropathy, guiding clinicians to the correct bedside diagnosis. NA involving the shoulders or spine suggests syringomyelia. NA of the feet and ankles suggests diabetes. Charcot arthropathy of the knees points to syphilis. Isolated hand NA suggests leprosy and, to a lesser extent, syringomyelia.
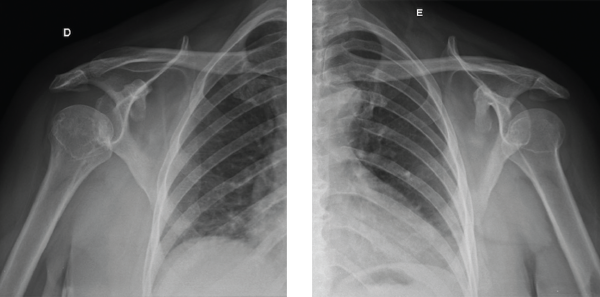
Figures 5A and 5B: These X-rays show incipient reabsorption of the ends of the humeri without the prominence of osteophytes and osteosclerosis.
Although many physicians expect further complementary exams to determine the type of neural injury, we believe a careful history coupled with a physical examination may correctly determine the essential exam physicians must perform, rather than using multiple electroneuromyography and whole-body MRI for the final diagnosis.
Zebras Do Exist!

Figure 6: This X-ray shows degenerative changes on the proximal and distal interphalageal joints and bone reabsortion at the fifth metacarpophalangeal joint of the left hand.
We generally agree with the saying, “When you hear hoofbeats, think horses, not zebras,” but we also teach medical students and fellows to be careful if they are at a safari—in this situation, hoofbeats may really be caused by zebras.
We presented this case to highlight the importance of vigilance on supposed RA patients’ refractory to synthetic disease-modifying anti-rheumatic drugs (sDMARDs), especially if they are seronegative and anchored on subjective complaints. Those cases should alert the physician to a possible RA mimicker, even in the presence of hand deformities.
In the absence of a perfect molecular disease activity marker, clinical acumen remains critical for dissecting patients’ complaints about pain and guiding treatment. Because pain is an abstract symptom, physicians must be aware of its different domains. Dr. Carlos Antonio Moura (one of the authors), tells his fellows that every time an RA patient seems to be failing a treatment regimen they should apply the mnemonic PAIN (see Table 1) to help them separate causes of pain and also to help them remember possible mimics and confounders of RA. Although it’s common for patients in the rheumatologist’s
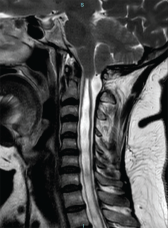
Figure 7: An MRI of the patient’s spine and head confirmed an extensive syringomyelia secondary to Chiari type I malformation.
office to present with an overlap of those different pain domains, it’s our job to dismantle them and find the best treatment strategies to avoid iatrogenic occurrences.
Other hand deformities may mimic RA as well, including nerve injuries (e.g., claw hand syndrome), mutilating psoriatic arthritis, erosive osteoarthritis, hemochromatosis (i.e., the so-called iron salute), Jaccoud arthropathy, calcium pyrophosphate deposition disease, tophaceous gout, multicentric reticulohistiocytosis and diabetic cheiroarthropathy.2
Bottom line: We think rheumatologists should know these conditions as well as they know RA.
Final Thoughts
Our case report illustrates a patient misdiagnosed with seronegative RA because of symmetric hand pain associated with atypical deformities. The presence of benediction hands plus Charcot arthropathy of shoulders and dissociated sensory loss on the upper extremities suggested a neuropathic origin of the disease, leading to the diagnosis of syringomyelia.
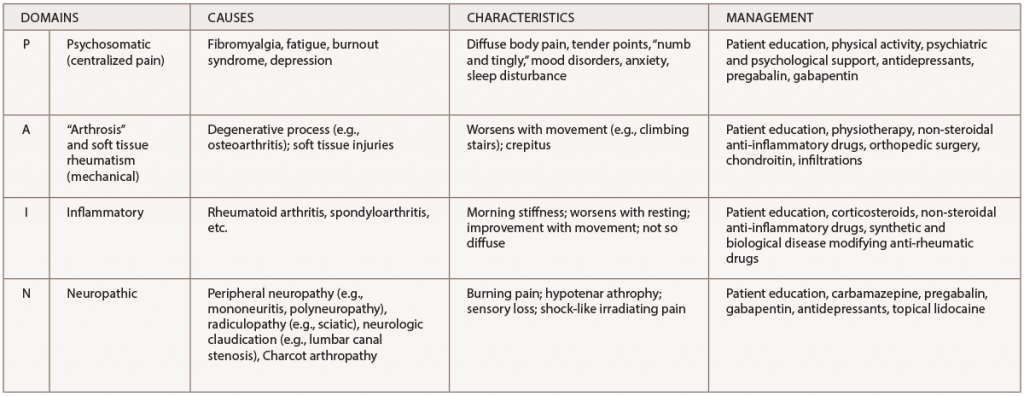
(click for larger image) Table 1: A Practical Approach to Pain Domains*
* It is not uncommon for patients in the rheumatologist’s office to present several of these pain areas concomitantly. It is our job to dismantle them to guide the best treatment decisions.
We hope this report helps other physicians remember that not all cases of symmetric hand pain and deformities are RA, especially when ACPA and RF are negative and the patient is refractory to first-line therapies.
 Carlos Antonio Moura, MD, is a rheumatologist and the preceptor of the internal medicine residency program at Hospital Santo Antônio in Salvador, Bahia, Brazil, and teaches at Salvador University and Escola Bahiana de Medicina e Saúde Pública.
Carlos Antonio Moura, MD, is a rheumatologist and the preceptor of the internal medicine residency program at Hospital Santo Antônio in Salvador, Bahia, Brazil, and teaches at Salvador University and Escola Bahiana de Medicina e Saúde Pública.
 Nathalia Crusoé, MD, is a resident in internal medicine at Hospital Santo Antônio in Salvador, Bahia, Brazil.
Nathalia Crusoé, MD, is a resident in internal medicine at Hospital Santo Antônio in Salvador, Bahia, Brazil.
 Marília Cruz, MD, is a resident in internal medicine at Hospital Santo Antônio in Salvador, Bahia, Brazil.
Marília Cruz, MD, is a resident in internal medicine at Hospital Santo Antônio in Salvador, Bahia, Brazil.
 Carlos Geraldo Moura, MD, is a rheumatologist and chief of the internal medicine residency program at Hospital Santo Antônio in Salvador, Bahia, Brazil, and teaches at Escola Bahiana de Medicina e Saúde Pública.
Carlos Geraldo Moura, MD, is a rheumatologist and chief of the internal medicine residency program at Hospital Santo Antônio in Salvador, Bahia, Brazil, and teaches at Escola Bahiana de Medicina e Saúde Pública.
References
- Mjaavatten MD, Bykerk VP. Early rheumatoid arthritis: The performance of the 2010 ACR/EULA criteria for diagnosing RA. Best Pract Res Clin Rheumatol. 2013 Aug;27(4):451–466.
- Lans J, Machol JA 4th, Deml C, et al. Nonrheumatoid arthritis of the hand. J Hand Surg Am. 2018 Jan;43(1):61–67.
- Neves, Fde S, Gonçalves DP, Gonçalves CR. Syringomyelia, neuropathic arthropathy and rheumatoid arthritis as diagnostic dilemmas in two different cases: confounding factor and true coexistence. Clin Rheumatol. 2007 Jan;26(1):98–100.
- Grear BJ, Rabinovich A, Brodsky, JW. Charcot arthropathy of the foot and ankle associated with rheumatoid arthritis. Foot Ankle Int. 2013 Nov;34(11):1541–1547.
- DeQuattro K, Imboden JB. Neurologic manifestations of rheumatoid arthritis. Rheum Dis Clin North Am. 2017 Nov;43(4):561–571.
- Bhattacharyya S, Helfgott SM. Neurologic complications of systemic lupus erythematosus, Sjögren Syndrome, and rheumatoid arthritis. Semin Neurol. 2014 Sep;34(4):425–436.