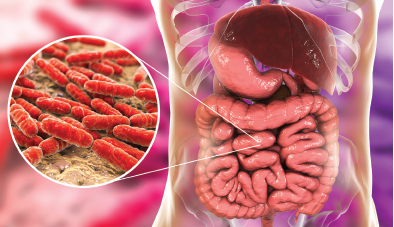
Kateryna Kon / shutterstock.com
CHICAGO—At the 2018 ACR/ARHP Annual Meeting, Allen C. Steere, MD, delivered the Rheumatology Research Foundation Memorial Lecture honoring the late Charles M. Plotz, MD: Linking Gut Microbial Immunity with Autoimmunity in Joints in Patients with Rheumatoid Arthritis. Dr. Steere is professor of medicine at Harvard Medical School, Boston, and director of translational research in rheumatology at Massachusetts General Hospital. His ongoing research focuses on the possible role of infectious agents in the microbiome, particularly Prevatella copri, in the initiation and perpetuation of pathogenic immune responses in rheumatoid arthritis (RA).
Bacterial Colonies in the Gut
Rheumatologists have made great progress in understanding RA’s genetic risk factors, but are only now identifying its environmental factors, said Dr. Steere. His lecture focused on the gut as a potential site of immune stimulation.
“Most of the microbiota is in the gut—more than 1,000 bacterial species and over 1 trillion bacterial cells,” he said. Dysbiosis, or a disruption of the normal balance in the microbial commensal ecosystem, with narrowing diversity, may result in disease.2 Gut dysbiosis has been demonstrated in rheumatic diseases like RA, ankylosing spondylitis, psoriatic arthritis and reactive arthritis. Implicated organisms in these diseases vary, but one common feature is reduction in diversity, allowing expansion of certain species.
“The hypothesis,” said Dr. Steere, “is that with narrowed commensal diversity, certain organisms are able to expand, attach to and invade the gut mucosa, where they promote an exaggerated immune response, activating systemic inflammation in a way that contributes to joint disease.”3
A 2010 study using K/BxN TCR transgenic mice showed the importance of segmented filamentous bacteria (SFB) and Th17 responses in arthritis development.4 These mice are engineered to develop arthritis as a response to glucose-6-phosphate isomerase (GPI). The study showed the mice did not develop arthritis in a germ-free environment, “but the introduction of SFB in germ-free mice was sufficient to reinstate Th17 cells, leading to the production of autoantibodies and arthritis, and neutralization of IL-17 prevented arthritis,” he said.
Humans do not have SFB. Can other organisms in humans’ microbiota induce this type of response? The answer is yes, said Dr. Steere. In a 2017 study, IgA-coated E. coli bacteria promoted Th17-dependent inflammation in patients with Crohn’s disease-related spondyloarthritis (SpA).5 They determined the identity of bacterial strains by 16S rDNA sequencing, and showed that only one bacterial taxon, E. coli Shigella, was significantly different between the two patient groups. E. coli were more often coated with IgA in patients with Crohn’s SpA than in those with just Crohn’s disease.
“What’s more, the height of the coating index to E. coli correlated with the BASDAI score in terms of the arthritis being more severe,” he said. Fifteen E. coli isolates from three patients were an invasive-adherent strain of the bacterium. Typically, commensal E. coli strains are neither adherent nor invasive. “Attachment and invasion of the organism to intestinal mucosa explains why the organism would activate Th17 responses.”
These authors conducted a study of KBxN mice and found that anti-GPI antibody titers were similar when the mice were inoculated with SFB or with the invasive-adherent E. coli strain isolated from the patients in the study. “This mouse is engineered to have autoantibody responses to GPI, but an organism implicated in human Crohn’s SpA, an invasive-adherent E. coli strain, was sufficient to cause Th17 responses and autoimmune arthritis in this model system,” Dr. Steere said.
Periodontitis & Autoimmunity
Dr. Steere
An epidemiological association exists between periodontitis and RA, and periodontal disease offers lessons on why RA patients may have autoantibody responses to citrullinated proteins, said Dr. Steere.
“In periodontitis, the gingival crevicular fluid becomes inflamed with polymorphonuclear leukocytes (PMNs) and matrix metalloproteinases (MMPs), and this favors certain anaerobic organisms that are able to flourish in an inflammatory environment,” he said. One particularly high-risk pathogen, Aggregatibacter actinomycetemcomitans (Aa), may cause severe periodontitis. Porphyrmonas gingivalis is another risky pathogen associated with gum disease. Research published in 2016 reveals that gingival crevicular fluid (GCF) showed extensive citrullination, mirroring the pattern of hypercitrullination of proteins seen in RA joints.6 Only P. gingivalis has a petidylarginine deiminase (PAD) enzyme that citrullinates arginines at the C-terminal portions of the protein, which may lead to immunoreactive neoepitopes, he said.7
However, the study’s authors “found that RA patients have citrullines in the middle portion of their proteins, as one would expect from citrullination caused by host PADs, not at the C-terminal ends, as with P. gingivalis PADs. They further showed that Aggregatibacter has a leukotoxin, which causes intracellular release of PADs from polymorphonuclear leukocytes. And only Aggregatibacter had the ability to produce a similar repertoire of citrullinated antigens in the GCF as in the RA joint.” It is important to learn whether such processes can play out in the gut, he said.
P. copri & RA
Other bacteria play a role in RA, especially P. copri. A 2013 study found overexpansion of Prevotella bacteria, especially P. copri, in the stool samples of 75% of patients with new-onset RA compared to a significantly smaller percentage of patients with chronic RA or healthy controls.8 P. copri expansion was at the expense of other species, such as Bacteroides, and particularly B. fragilis, which may be important in T-regulatory cell development and function, said Dr. Steere.
A 2016 study conducted in Japan showed that Prevotella, particularly P. copri, dominated one cluster of fecal microbiota from RA patients.9 These researchers then analyzed SKG mice, which have a point mutation in the ZAP-70 gene that leads to defective T cell selection in the thymus. These mice develop Th17-cell-dependent arthritis, but do not develop disease in a germ-free facility. After treatment with zymosan, SKG mice inoculated with Prevotella-dominant feces from RA patients showed increased numbers of Th17 intestinal cells and developed more severe arthritis.
Dr. Steere and his colleagues are studying immune responses to P. copri and novel autoantigens in an effort to link gut microbial immunity with autoimmunity in joints. They developed a discovery-based approach to identify important microbial or self-antigens in RA and in antibiotic-refractory Lyme arthritis based on the identification of HLA-DR-presented peptides from synovial tissue, synovial fluid mononuclear cells (SFMC) or peripheral blood mononuclear cells (PBMC) using nano-tandem mass spectrometry.10 They determined the antigenicity of each peptide by stimulating the matching patient’s PBMC with each peptide in ELISpot assays.
Test results from one female RA patient was of particular interest, he said. She had classic symmetrical polyarthritis and two copies of shared epitope alleles. However, she had a negative result for both rheumatoid factor and anti-CCP antibodies until three years into her disease, when she had first tested positive for anti-CCP.
“She had a good response to DMARD therapy, except for one knee, which remained inflamed,” he said. For this reason, they performed arthroscopic synovectomy of this knee and analyzed her synovial tissue, synovial fluid and peripheral blood for immunogenic HLA-DR-presented peptides, or T cell epitopes. From her synovial tissue, they identified 124 non-redundant HLA-DR-presented peptides from 86 source proteins. Only two peptides were immunoreactive: N-acetylglucosamine-6-sulfatase (GNS) and filamin A (FLNA). “Neither of these proteins were previously described as auto-antigens in RA,” he said. They found 19 non-redundant peptides in her synovial fluid, but none were immunoreactive. From her PBMC, they identified two immunoreactive peptides. One was derived from a P. copri protein, which they called Pc-p27, and the other was a self-peptide derived from FLNA, the same T cell epitope found in her synovial tissue, he said.
In a 2017 study, Dr. Steere and his colleagues looked for T and B cell responses to Pc-p27 in RA patients.11 In patients’ PBMC samples, they found 42% of new-onset RA patients had T cell reactivity with the Pc-p27 peptide. In addition, 32% of patients with new-onset RA or chronic RA had antibody responses to Pc-p27 and/or whole P. copri lysates. One subgroup had IgA antibody responses to P. copri, which correlated with Th17 responses and ACPAs, which suggested a mucosal immune response. The other subgroup had IgG antibodies to P. copri, which were associated with Prevotella DNA in their synovial fluid, P. copri-specific Th1 responses and, less frequently, ACPAs, which suggested a systemic immune response.
They also tested two autoantigens, GNS and FLNA, and found that 52% of RA patients had T cell responses, and 56% had antibody responses to one or both of these antigens.12 “The reactivity with these microbial and self-antigens was significantly more common in patients with shared epitope alleles, as one might expect, since these T cell epitopes were originally identified in a patient with two copies of shared epitope alleles,” said Dr. Steere.
The GNS protein appeared to be citrullinated in vivo, while the FLNA protein did not. GNS antibody levels correlated with ACPA levels, but FLNA antibody levels did not. With both GNS and FLNA, reactivity was seen primarily around the blood vessels in the synovial tissue of RA patients.
“This is common in autoimmune diseases, that reactivity with auto-antigens often occurs around blood vessels. It raises the question of whether this is an early pathological response that is important in what then happens downstream,” he said.
P. copri IgA responses in RA joints, but not P. copri IgG responses, also correlate with two Th1 cytokines in patients’ serum, IFNγ and IL-12, and even more dramatically, with three Th17 cytokines, IL-17, IL-22 and IL-1β, said Dr. Steere.
“These correlations suggest that inflammation may also occur outside the joint, and I’ll postulate that this happens within the bowel mucosa, consistent with the importance of the Th17 response in the pathogenesis of autoimmune disease.”
Gut Dysbiosis–Joint Links
What is the link between immune responses in RA patients’ gut mucosa and what is happening in their joints? One hypothesis is that T cell epitope mimicry between microbial proteins in patients’ guts and the host proteins in their joints trigger cross-reactive, autoimmune responses that affects their joints, said Dr. Steere.
The National Institutes of Health (NIH) database on T cell epitopes from human and microbial sources shows that up to six of the nine amino acids in the HLA-DR-binding groove commonly overlap between human and microbial proteins. However, cross-reactive T cell epitopes are more common between human proteins and commensal bacterial proteins than with pathogenic bacteria, he said. This suggests many foreign epitopes would be recognized by self-reactive T cells.13
“Why would there be more T cell epitope mimicry between host proteins and those of commensal organisms than with those of pathogens?” asked Dr. Steere. It may relate to the importance of generating T-regulatory cells. “However, one could also hypothesize, that under certain circumstances, due to the plasticity of the Th-cell repertoire, that some T-reg cells may become Th17 cells that have a pathologic function.”
Dr. Steere’s laboratory’s research found that the GNS peptide had a 67% sequence homology with a Prevotella aryl-sulfatase protein, and these peptides share amino acid identity at the P1, P4 and P6 sites. They also found the FLNA peptide had 80% sequence homology with a secreted Prevotella protein, with seven of nine identical amino acids in the binding groove.14 They found T cell reactivity to both the GNS peptide and the related Prevotella peptide in about one-third of RA patients.
These patients often reacted with a similar epitope of a sulfatase protein of Parabacteroides species. About one-third of RA patients had T cell reactivity to both the FLNA sequence and the related Prevotella sequence, and to a similar sequence in Butyricimonas.
In each case, the higher the T cell reactivity to the microbial peptide, the higher the response to that self-peptide. They also found positive correlations between patients’ IgG and IgA P. copri antibodies, and their GNS or FLNA antibodies, a correlation not seen with P. gingivalis antibodies, he said.
“Our second hypothesis was based on the finding of Prevotella DNA in joint fluid in some patients with IgG P. copri antibodies. We hypothesized that P. copri or its remnants may spread directly to joints, presumably within cells. It’s an anaerobe, so it’s not going to survive well in the bloodstream in an aerobic environment,” he said. “Perhaps P. copri or its components may reach the joints in APCs [antigen-presenting cells], where they could stimulate joint inflammation.”
Past research has shown PCR positivity for the DNA of various bacterial organisms in the joints of patients with RA, reactive arthritis or osteoarthritis, said Dr. Steere.
“It’s been hard to know what to make of that. Is it simply an epiphenomenon? One has this image of DNA from the bowels floating around systemically and then occasionally getting into the joints.” He and his colleagues conducted nested PCR testing of matched samples of serum joint fluid from 18 RA patients. Importantly, they detected Prevotella 16S DNA in the synovial fluid of three patients, and found that they had IgG antibody responses to P. copri.
“What’s different here is the clinical correlation between P. copri DNA in joints and P. copri IgG antibody responses, which suggests this may be more than an epiphenomenon,” said Dr. Steere. “Those three patients were among the five who had IgG antibody responses to P. copri. We did not find this in the patients with IgA responses or in those who were negative for P. copri antibody responses.”
When the PCR products from the three patients were sequenced, each had a slightly different sequence, which may be explained by the fact that each patient grew up in a different geographic region. Different sequences show this result could not be explained by cross-contamination among the three samples, he said.
Although this hypothesis seems bold, bacteria–inflammation links are found in other diseases, including cancer, said Dr. Steere. A 2013 study showed that a commensal anaerobe found in the oral cavity implicated in periodontal disease, Fusobacterium nucleatum, has the potential to spread, bind to adenomatous polyps in the bowel, and induce inflammatory and oncogenic changes, leading to colorectal adenocarcinoma cells. In a mouse model, an inhibitory 11 amino acid peptide blocked this binding and prevented oncogenesis.15
Rheumatologists should consider the implications of these findings for future diagnosis and treatment of RA, he concluded.
“Will we someday need to determine a site of mucosal involvement in patients with new-onset RA? And the earlier, the better? Will we test not just for rheumatoid factor and ACPA, but also for antibody responses to certain commensals and/or related auto-antigens? I suspect that the answer is yes,” said Dr. Steere.
Patients with gut-associated antibody responses might be treated not only with DMARDs, but with directed antibiotics, probiotics or diet to restore normal commensal balance in their bowels. “Will we someday be able to target pathogenic microbial or host T cell epitopes using blocking peptides? Identification of pathogenic T cell epitopes, which may require precision medicine, may make this possible.” This strategy has shown encouraging results in several allergic and autoimmune diseases, he said.16
Dr. Steere closed by acknowledging the contributions of several co-investigators to this ongoing research, including Drs. Annalisa Pianta, Klemen Strle, Catherine Costello and Elise Drouin.
Susan Bernstein is a freelance medical journalist based in Atlanta.
References
- Plotz CM, Knowlton AI, Ragan C. The natural history of Cushing’s syndrome. Amer J Med. 1952;13;597–614.
- Rosenbaum JT, Silverman GJ. The microbiome and systemic lupus erythematosus. N Engl J Med. 2018 Jun;378:2236–2237.
- Scher JU, Abramson SB. The microbiome and rheumatoid arthritis. Nat Rev Rheumatol. 2011 Aug 23;7(10):569–578.
- Wu HJ, Ivanov II, Darce J, et al. Gut-residing segmented filamentous bacteria drive autoimmune arthritis via TH helper 17 cells. Immunity. 2010 Jun;32(6):815–827.
- Viladomiu M, Kivolowitz C, Abdulhamid A, et al. IgA-coated E. coli enriched in Crohn’s disease spondyloarthritis promote Th17-dependent inflammation. Sci Transl Med. 2017 Feb;9(376):pii: eaaf9655.
- Konig MF, Abusleme L, Reinholdt J, et al. Aggregatibacter actinomycetemcomitans-induced hypercitrullination links periodontal infection to autoimmunity in rheumatoid arthritis. Sci Transl Med. 2016 Dec;8(369).
- Wegner N, Wait R, Sroka A, et al. Petidylarginine deiminase from Porphyrmonas gingivalis citrullinates human fibrinogen and α-enolase: Implications for autoimmunity in rheumatoid arthritis. Arthritis Rheum. 2010 Sep;62(9):2662–2672.
- Scher JU, Sczesnak A, Longman RS, et al. Expansion of intestinal Prevotella copri correlates to enhanced susceptibility to arthritis. eLife. 2013 Nov 5;2:e01202.
- Maeda Y, Kurakawa T, Umemoto E, et al. Dysbiosis contributes to arthritis development via activation of autoreactive T cells in the intestine. Arthritis Rheumatol. 2016 Nov;68(11):2646–2661.
- Wang QI, Drouin EE, Yao C, et al. Immunogenic HLA-DR-presented self-peptides identified directly from clinical samples of synovial tissue, synovial fluid or peripheral blood in patients with rheumatoid arthritis or Lyme arthritis. J Proteome Res. 2017 Jan;16(1):122–136.
- Pianta A, Arvikar S, Strle K, et al. Evidence of the immune relevance of Prevotella copri, a gut microbe, in patients with rheumatoid arthritis. Arthritis Rheumatol. 2017 May;69(5):964–975.
- Pianta A, Arvikar S, Strle K, et al. Two rheumatoid arthritis-specific autoantigens correlate microbial immunity with autoimmune responses in joints. J Clin Invest. 2017 Aug 1;127(8):2946–2956.
- Rose NR. Negative selection, epitope mimicry and autoimmunity. Curr Opin Immunol. 2017 Nov;49:51–55.
- Pianta A, Arvikar S, Strle K, et al. Two rheumatoid arthritis-specific autoantigens correlate microbial immunity with autoimmune responses in joints. J Clin Invest. 2017 Aug 1;127(8):2946–2956
- Rubinstein MR, Wang X, Liu W, et al. Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating E-cadherin/β-catenin signaling via its FadA adhesin. Cell Host Microbe. 2013 Aug;14(2):195–206.
- Larche M, Wraith DC. Peptide-based therapeutic vaccines for allergic and autoimmune diseases. Nat Med. 2005 Apr;11(4 Suppl):S69–S76.


