“That was a big change, in terms of patient access,” Dr. Bowman says. “Suddenly, the hospitals had to collect data and make sure patients were booked in the 12-week timeframe. It made a very big difference to outpatient specialties like rheumatology, dermatology, etc.”
Even with regulation, a recent report showed “unacceptable” wait times for rheumatoid arthritis and psoriatic arthritis patients in the U.K. The research showed a 10% increase in “unacceptable delays” of 12 weeks or more to see a specialist in the past 10 years.2
“It is true that in many areas the time (from referral to specialist visit) is slipping a little bit,” Dr. Bowman says. “But the data probably should be taken with caution. Things are much improved over the past 10–15 years. On the whole, there probably are regional variations. In my locality, rheumatologists are able to meet these ideals.”
Meeting the “window of opportunity” target is reliant on all cogs in the health system wheel functioning correctly, Dr. Bowman says. Nurses and support staff, positions that are first to be cut in times of economic downturn, are critical to follow-up care. Another key is continued education for patients and referring physicians.
“In this country, our focus is on new patients, instead of follow-up,” he says. “That can have an impact on subsequent care. That can be somewhat challenging, and it’s complex. In Europe, my colleagues are expected to see fewer patients than in the U.K., and are expected to spend more time with follow-up. Probably at the moment, there is not a great deal of prospect for that to be modified.”
The U.K. is dealing with similar obstacles to patient access in the U.S., in terms of an aging population, workforce capacity and government cuts to budgets, says Alan J. Silman, MD, medical director of Arthritis Research UK.
“The issue here is what part of the workload can be handled in primary care, particularly for non-inflammatory joint disease, including osteoarthritis, back pain and fibromyalgia,” says Dr. Silman, who notes new initiatives, such as the “best practice tariff” and “treat to target,” allow for patients with newly diagnosed inflammatory arthritis to be seen and started on treatment quickly. “There are a number of models being developed, with closer integration of primary and secondary care, including, for example, development of skilled physiotherapist and other healthcare professionals who can manage many of these patients.”
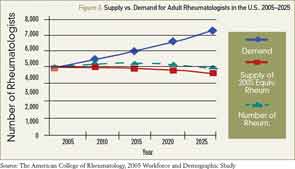
Source: The American College of Rheumatology, 2005 Workforce and Demographic Study
The Numbers
In 2005, the ACR published research that showed demand for rheumatologists in 2020 would be about 6,500, but only slightly more than 5,000 rheumatologists would be in active practice. By 2025, the gap was projected to widen to 2,000 (see Figure 2).