Howard Blumstein, MD, realizes the U.S. system is headed for “a real problem” and is concerned about the impact the Affordable Care Act will have on patient-access issues.
“The future here is extremely hazy,” says Dr. Blumstein, a partner in Rheumatology Associates of Long Island, N.Y. “I wonder how much the [U.K.] model will [translate] here, where we will become managers of armies of nurse practitioners or physician assistants doing the day-to-day work. Personally, that’s not why I went into this field. To me, that’s scary stuff.”
Changes in workforce demographics and productivity are generational, Dr. Blumstein says. He says it’s hard to argue with newly minted doctors choosing work-life balance or taking a secure salary in a hospital-employed position.
Dr. Huffstutter, whose daughter is in medical school, realizes that more women in medicine—about 60% of rheumatology trainees are women—will affect patient access in the future.
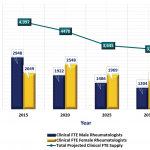
“This is a gender-shift issue in medicine,” Dr. Battafarano says. “It is conceivable that a subset of female physicians, for a variety of reasons, will practice part time at some point in their career. We may be graduating and training more rheumatologists in 2014 than we were in 2000, but the gender shift definitely will influence access to rheumatology care. This is not unique to rheumatology, but is true for other subspecialties as well.”
Short-Term Fix
No single solution will fix patient-access issues in the U.S., experts agree. Some say, “Train more rheumatologists.” Some say rheumatologists need to do a better job educating primary care and patients on the importance of early diagnosis and referral. Others, but not all, think that easing limitations on nurse practitioners (NPs) and physician assistants (PAs) is a good place to start. But everyone seems to agree that those are only pieces of the larger puzzle.
“In my opinion, the biggest short-term solution for rheumatology access is training more NPs and PAs,” Dr. Battafarano says. “That would require us to recruit them into the rheumatology profession, and it would require us to have more formal training programs—in addition to training some in private practice settings. Longer-term solutions to improve access include recruiting rheumatology providers to underserved areas and better training for [primary care physicians] to recognize and treat RA early.”
Richard Quinn is a freelance writer in New Jersey.
References
- Department of Health. The NHS Plan: A plan for investment, a plan for reform. London: Department of Health, 2000. July 1, 2000. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4002960.
- More rheumatoid arthritis and psoriatic arthritis patients waiting “unacceptable” times for referral than a decade ago. Business Wire website. Jan. 29, 2014. http://www.businesswire.com/news/home/20140129005500/en/Rheumatoid-Arthritis-Psoriatic-Arthritis-Patients-Waiting-%E2%80%9CUnacceptable%E2%80%9D#.U1A-ZBlRE5N.